Intranodular hyperechogenic figures - case 195 |
|
Clinical presentation: A 37-year-old woman requested a second opinion. She suffered from fluctuating periods of hypothyroidism and hyperthyroidism for more than 2 years. Despite great efforts including steroid therapy, combination of replacement and thyrostatic therapy and unusually frequent follow-up examinations (checking hormone-levels every 2 to 4 weeks) to maintain euthyroid state, the patient presented alternating severe hypothyroidism and hyperthyroidism within several weeks. The patient lost her patience because she wanted to be pregnant. It is worth noting that TSAb levels were repeatedly undetectable, while aTPO was in the range of 150 to more than 1,000 U/mL.
Palpation: no abnormality.
Functional state: euthyroidism on daily 50 microgram levothyroxine (TSH 3.09 mIU/L, FT4 20.2 pM/L, aTPO 243 U/mL).
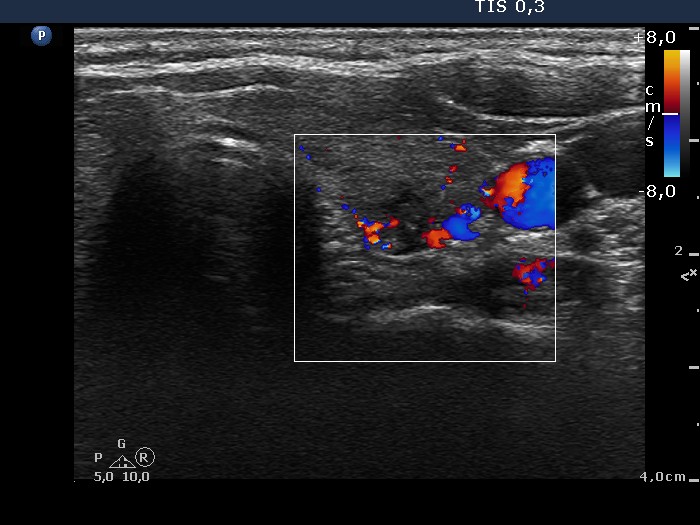
Ultrasonography: The thyroid was hypoechogenic. There was a small, more hypoechogenic area with blurred borders and a focus of microcalcification in the left thyroid.
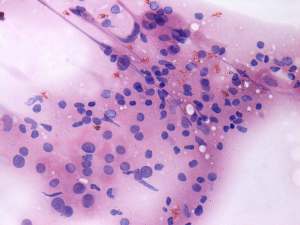
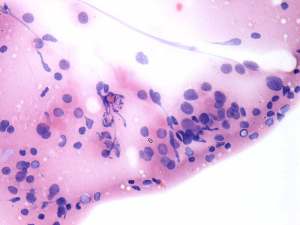
Cytology was performed from the lesion in the left lobe and resulted in Hashimoto's thyroiditis.
In order to maintain a stable thyroid state total thyroidectomy was advised.
Histopathology disclosed Hashimoto's thyroiditis without any nodule.
Comment. The patient had a long lasting, clinically subacute, pathologically lymphocytic thyroiditis for more than 3 years. It is a very rare situation. In our practice with ten-thousands of patients with autoimmune thyroiditis, we have found not more than 10 patients whose clinically subacute, pathologically lymphocytic thyroiditis did not resolve within 18 months. Total thyroidectomy is the resolution in such patients.