Chronic lymphocytic thyroiditis - Case 71. |
|
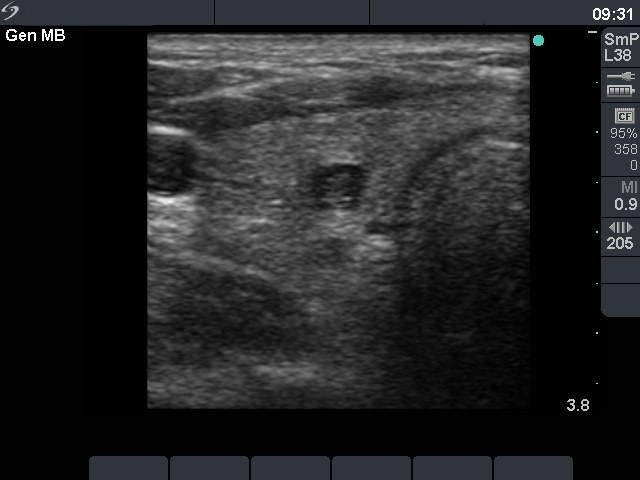
First examination on 16th gestational week (first row):
Clinical presentation: a 31-year-old woman was referred for an evaluation of a suspected hyperthyroidism. She had hyperemesis gravidarum.
Palpation: no abnormality.
Functional state: euthyroidism with subnormal TSH-level: TSH 0.12 mIU/L, FT4 20.2 pM/L, FT3 4.01 pM/L.
Ultrasonography: the thyroid was echonormal with an insignificant lesion in the right lobe.
We advised a repeated hormonal investigation 8 weeks later which resulted in euthyroidism with TSH 0.91 mIU/L, FT4 18.2 pM/L.
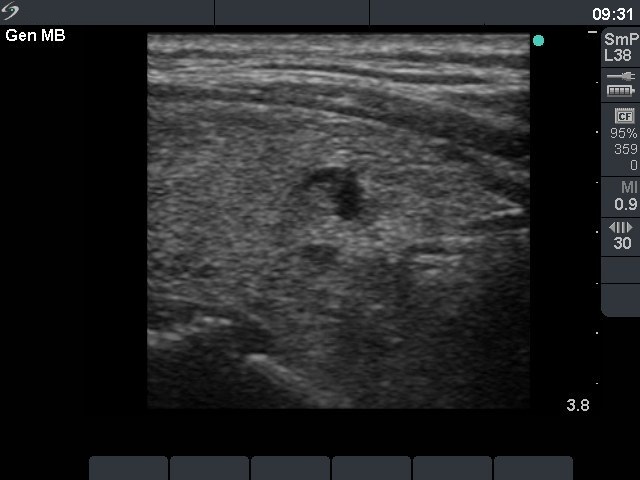
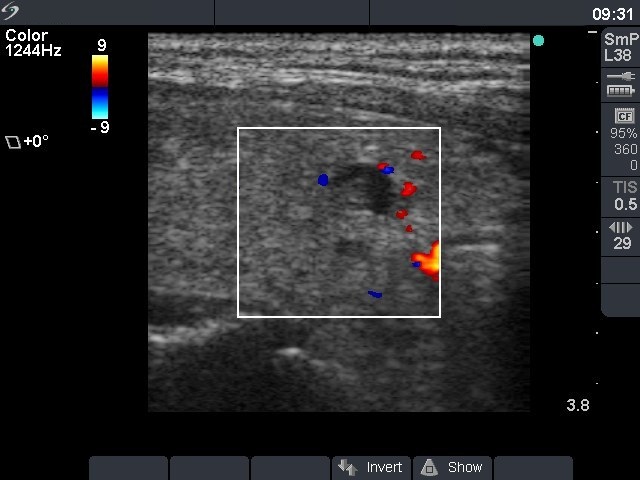
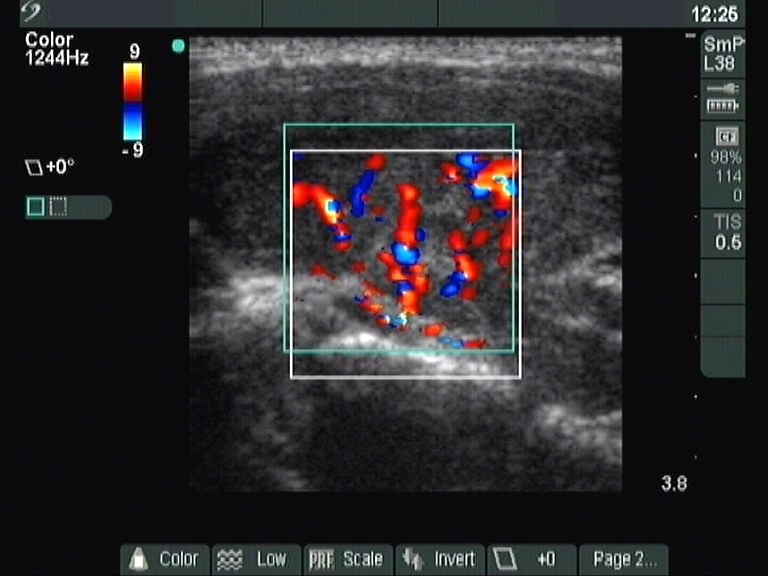
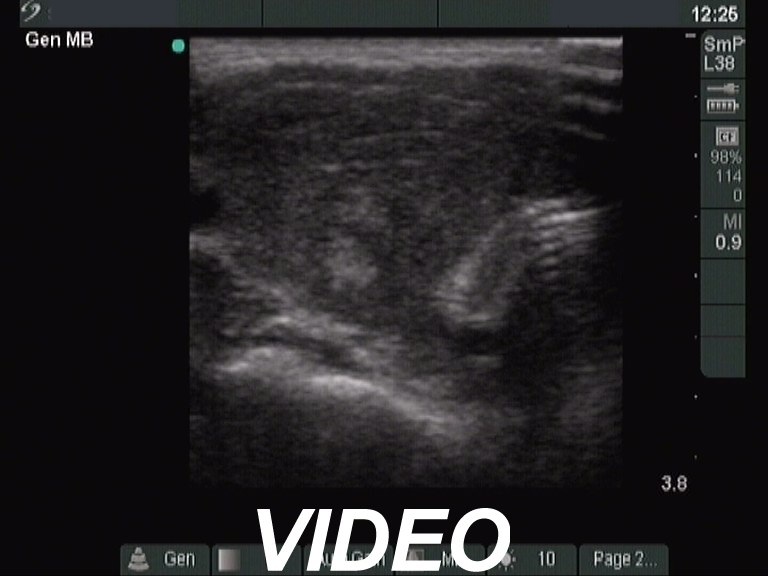
Follow-up examination 7 weeks after delivery (second row):
Clinical presentation: the patient visited us because of typical clinical signs of hyperthyroidism.
Palpation: the thyroid was enlarged and firm.
Functional state: hyperthyroidism with TSH-level 0.001 mIU/L, FT4 43.3 pM/L, FT3 9.01 pM/L.
Ultrasonography: the thyroid was enlarged and hypoechogenic. The vascularization was increased.TSH-antibody test was negative (below 0.1 U/L) while anti-TPO was elevated 605 U/mL.
Diagnosis: hyperthyroidism caused by post partum thyroiditis. We did not suggest any drugs.
On a follow-up investigation 6 weeks later, the FT4 level had normalized (13.3 pM/L). Two months later hypothyroidism developed with TSH 28.0 mIU/L, FT4 6.09 pM/L. Four months later a gradual normalization was observed with TSH 13.3 mIU/L, FT4 13.9 pM/L.
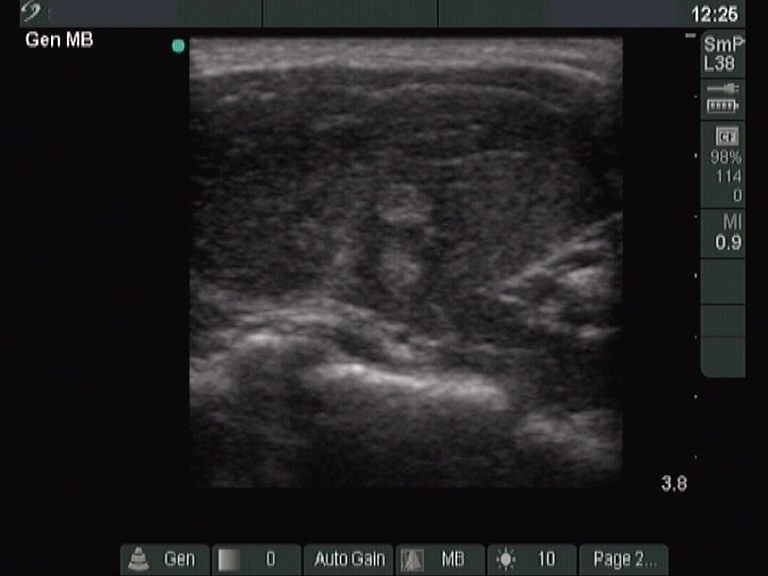
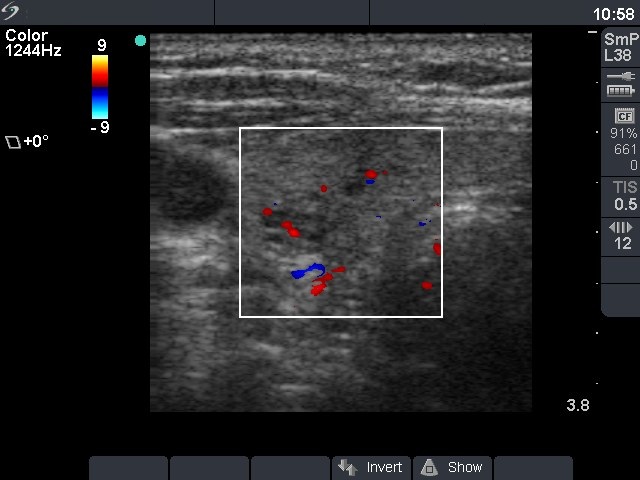
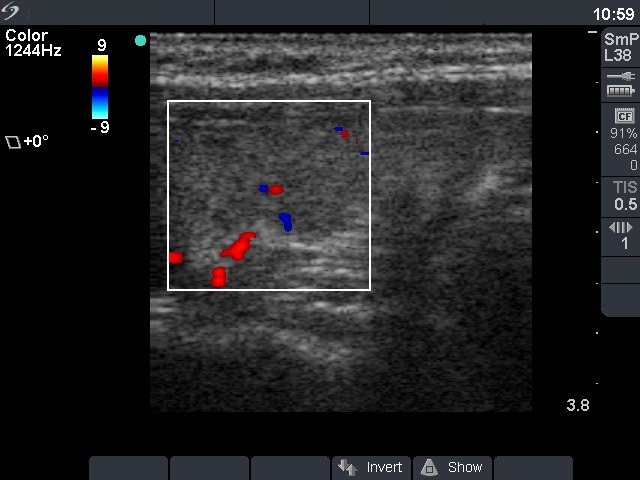
Follow-up investigation 16 months after delivery (third row):
Clinical presentation: the patient had no complaints except for moderate degree of fatigue.
Palpation: no abnormality.
Functional state: euthyroidism with TSH-level 3.02 mIU/L, FT4 14.6 pM/L.
Ultrasonography: the echo structure was normal with around 10% of the hypoechogenic areas. The vascularization was normal.
Suggestion: TSH determination every year, in the case of pregnancy at once.
Comments:
-
This case is an example of a typical biochemical and ultrasound course of post partum thyroiditis. By chance we could evaluate the patient earlier, therefore we could demonstrate that the thyroids seemed healthy before the post partum period.
-
In the first 3 months of pregnancy, a subnormal TSH (between 0.1-0.4 mIU/L) must not be judged as abnormal.