|
Graves' disease |
|
Clinical presentation and ultrasonography
Most considerations made in the section about lymphocytic thyroiditis are valuable in the case of Graves' disease. The difference between the two autoimmune diseases is mainly not in the US presentation but the practical-clinical presentation. Nowadays, the diagnosis of LT is made by chance. Great proportion of the patients has no special complaints, but was investigated simply on screening or because of the suspicion of a nodular goiter. It means that the physician is not aware of clinical data, hormonal status etc.
The clinical situation greatly differs in a Graves' patient. These patients have complaints and in most cases we are aware of the clinical diagnosis when we perform US. It is worth describing why we prefer US in a patient with an unequivocal Graves' disease at all. Firstly, the size of the thyroid is of prognostic value and it influences whether a definitive or a conservative therapy is the choice. Secondly, the patient may also have a thyroid nodule, and it would be a failure to overlook this coincidence in a patient who has been treated for months or even years.
The performance of US is mandatory in a hyperthyroid patient without TAO. We can immediately determine whether the hyperthyroidism is caused by a nodular or a diffuse thyroid disease. If we diagnose a nodule, scintigraphy is mandatory in order to prove or exclude a toxic nodular goiter. If we do not see a nodule on US, the vascularization of the thyroid may be of diagnostic value. As described earlier, a decreased vascularization practically excludes the possibility of a hormone-producing disorder and this pattern greatly increases the possibility of the so-called hashitoxicosis.
The basic ultrasound property of the acute phase of Graves' disease is the hypoechogenicity. The degree of hypoechogenicity has very limited significance. The vascularization is increased in the early phase.
The correct interpretation of a discrete lesion is also a problem in Graves' disease. As mentioned earlier, the situation is not as difficult as in the case of LT, because in most cases we are aware of the clinical diagnosis. The second favourable circumstance can be explained by the more rapid change in the US pattern. If we have doubt about the origin of a lesion, a repeat ultrasound 3 or 6 months later may resolve the issue. The basic hypoechogenic pattern in most cases moves to a less hypoechogenic one. This relatively rapid modification in the ultrasound is of help to recognize a hypoechogenic nodule missed during the first US examination because of the similarity in the echo pattern of the nodular and non-nodular parts of the thyroid.
The US has prognostic value not only in the initial phase but also later in the course of the disease. If the hypoechogenic pattern and the increased blood flow are not decreased within one year after the therapy, then the recurrence rate is significantly higher. These US properties have similar prognostic value as the TSH-receptor antibody determination.
Cytology
Essentials
In this chapter, we discuss different entities which share a common cytological appearance. These clinical entities are as follows:
- Graves-Basedow's disease (current or previous treatment with thyrostatic drugs)
- Patients who have received previous I-131 therapy for hyperthyroidism
- Patients presenting with serious hypothyroidism
Besides the common cytological picture, there is another common feature of these entities: we can be aware of the previous or present hormonal dysfunction of the thyroid.
Indications for FNAC of goiter with a thyroid dysfunction
1. Hyperthyroid patients
without a thyroid nodule The underlying disease is not evident: it
could be Graves-Basedow's disease or Hashimoto's thyroiditis. In rare
cases, even subacute thyroiditis should be considered.
2. A thyroid nodule is present either in patients with hyperthyroidism
or in those previously treated for hyperthyroidism. The prevalence of
thyroid carcinoma in the presence of hyperthyroidism is reported to be
0.5% to 21.5% ( Krause 1991 ).
Typical cytological presentation
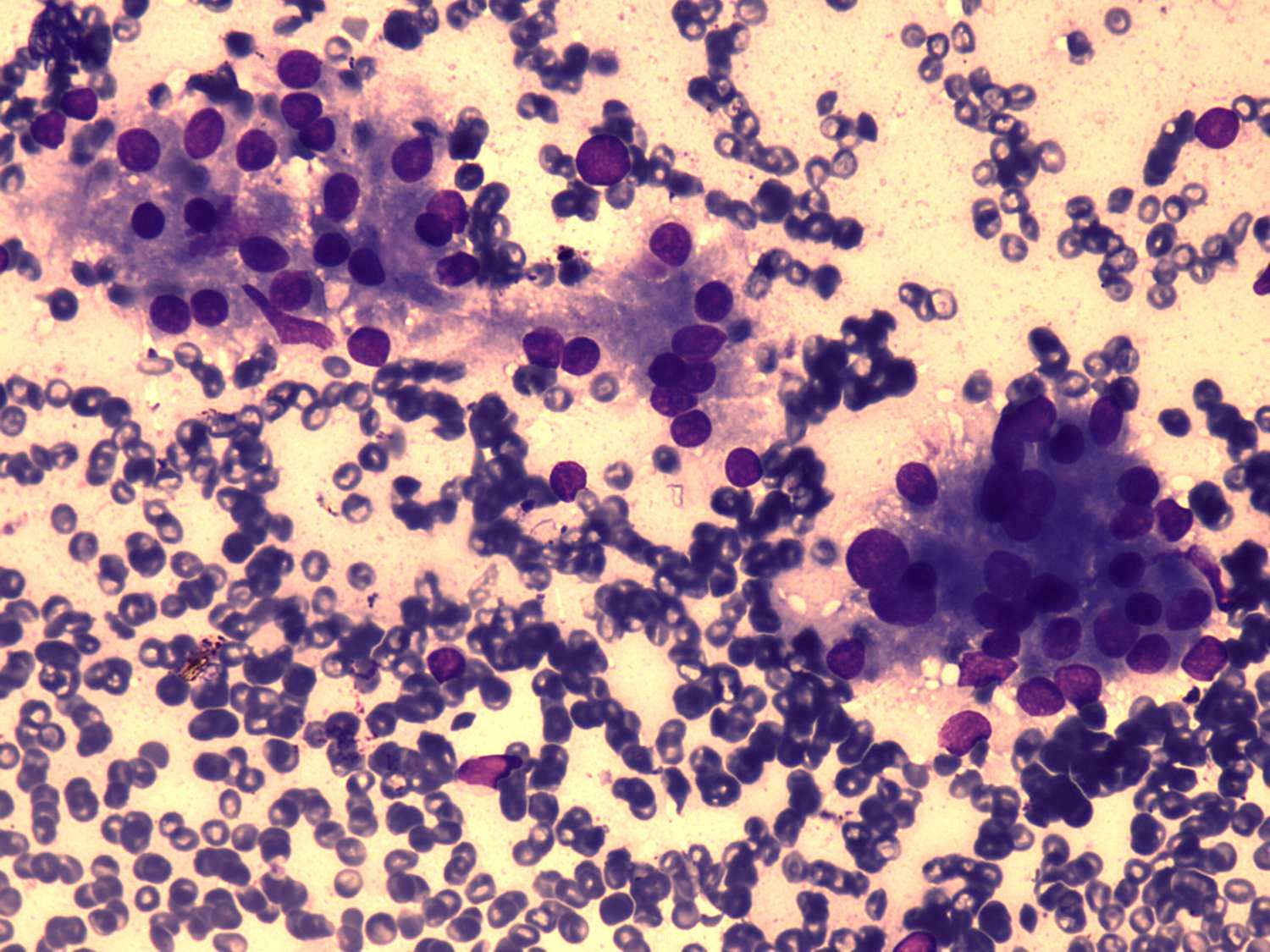 The smears
are bloody, and there is no or only minimal colloid in the background.
The smears
are bloody, and there is no or only minimal colloid in the background. - Marginal vacuolization (the fire flare appearance).
- The cells are round, with marked anisonucleosis.
- The cells are arranged in loose groups, and a follicular pattern (mostly formed by 6-10 cells) is also present.
None of the above-mentioned signs is pathognomic for Graves-Basedow's disease. The marginal vacuoles represent dilated cisternae of the endoplasmatic reticulum (Jayaram 1989a). This phenomenon occurs even in euthyroid goiters and lymphocytic thyroiditis, and also in carcinomas ( Nilsson 1972, Jayaram 1989a, Pitts 1989 ). Only rarely have we observed colloid in the hyperthyroid state of the disease, whereas others have found scanty, weakly stained colloid in half of their cases Droese 1995). A very characteristic sign is the round shape of the cell. Even highly enlarged cells demonstrate this feature.
Is there a nodule?
Before a discussion problematic cases, one basic problem must be answered. Both before and after the analysis of a cytological pattern that is difficult to interpret, we must be aware of whether the patient has a nodule or not.
The problem lies in the difficulty of the clear-cut diagnosis of a thyroid nodule in Graves-Basedow's disease. If a nodule is palpated and at the site of the nodule there is a discrete echo abnormality, then the presence of the nodule is no longer questionable. In contrast, in cases where no nodule is palpable, or in cases of palpable nodules without discrete echo abnormalities, the presence of a nodule is questionable. The problem lies in the fact that the US pattern of hyperthyroidism itself is hypoechogenic and most thyroid nodules are also hypoechogenic. Moreover, most US patterns outside the nodule in Graves-Basedow's disease change their characteristics over a period of months.
The latter phenomenon may be of help in resolving the problem. The echo structure of the thyroid has begun to normalize in around two-thirds of the patients at 6 months, and in around four-fifths of them at 12 months, and a nodule can be therefore visualized more easily on a second US investigation. If we perform repeated US in most of the cases where there is an initial doubt as to whether to diagnose a nodule or not, a clear-cut resolution can be made. The US follow-up of Graves-Basedow's patients is of great relevance in another case. The detection of a hypoechogenic nodule at the time of diagnosis of Graves-Basedow's disease may be very difficult or even impossible. Both 2 false-negative cases where a nodule larger than 5 mm in diameter was not detected by US occurred in patients with Graves-Basedow's disease. This led us to change our former practice, and in all of our patients with Graves-Basedow's disease we now perform repeated US 6-monthly until the US pattern of the thyroid normalizes in order to detect a nodule with a US pattern identical to that initially presented for the whole thyroid in Graves-Basedow's disease.
Cases that are difficult to interpret
| What to see? | What to think? |
| 1. A marked follicular proliferation | Is it a follicular tumor? |
| 2. The cells are not round | Could it be a tumor? |
| 3. The cells form papillary fragments | Can we rule out papillary cancer? |
| 4. Nuclear inclusions or grooves are present | Is it papillary cancer? |
| 5. There are numerous lymphocytes in the smear | Is it lymphocytic thyroiditis? |
Differential diagnostics in detail
Follicular proliferation
On the basis of the
cytological picture, a follicular tumor cannot be ruled out if a marked
follicular proliferation is present. Well-differentiated thyroid tumors may take part in the
enhanced hormone production observed in Graves-Basedow's disease. Thus,
other cytological signs of hyperthyroidism (vacuolization and
anisonucleosis) are of no relevance in the differential diagnostics.
present. Well-differentiated thyroid tumors may take part in the
enhanced hormone production observed in Graves-Basedow's disease. Thus,
other cytological signs of hyperthyroidism (vacuolization and
anisonucleosis) are of no relevance in the differential diagnostics.
In cases of the nodular form of hyperthyroidism, scintigraphy must be performed except when there is a clear-cut indication for surgery (a large thyroid with compression signs). If scintigraphy reveals a hot nodule in the area in question, the cytological problem is resolved: the patient has a toxic nodule, which in more than 95% of the cases is a follicular adenoma. In this clinical situation, either I-131 therapy or surgical removal of the nodule is the treatment of choice.
On
the other hand, if a patient does not have a toxic nodule in the area
in question, or the isotope uptake of the nodule is not evaluable,
because the nodule lies in the dorsal part of the thyroid, the
differential diagnostic problem remains to be resolved. This situation
does not differ essentially from that in nodular goiter with a
cytological picture of follicular proliferation. The only difference
lies not in the cytological differentiation, but in the fact that in
patients with a hyperthyroidism and with suspicion of a follicular
tumor there are two independent features favouring a surgical procedure
as the treatment of choice.
Cellular atypia: nuclear pleomorphism
 When we
see nuclei with an irregular shape, the possibility of an underlying
tumor must be excluded. There is no other disease in the thyroid where
the round shape of the cell is so characteristic. In a retrospective
analysis, more than 95%
of Graves-Basedow's disease cases without tumor were characterized via
the round shape (nuclear form factor < 1.15). On the other hand, in
more than 70% of cases where this factor was greater than 1.2, a tumor
was present. Accordingly, if a significant number of the cells are oval
or irregular in shape, other signs of a
potential thyroid tumor must be looked for with great thoroughness. If
other unusual signs are present, the possibility of a tumor must be
considered. In one of our false-negative case, only the oval shape of
the cells and the presence of macrophages could be noted on
hematoxylin-eosin and Giemsa-stained smears at the first cytological
investigation. The original report was benign. 2 years later, when
repeated FNAC was performed and we applied the Papanicolau method for
staining, nuclear grooves could also be observed and the patient was
sent for operation: histopathological examination revealed papillary
cancer.
When we
see nuclei with an irregular shape, the possibility of an underlying
tumor must be excluded. There is no other disease in the thyroid where
the round shape of the cell is so characteristic. In a retrospective
analysis, more than 95%
of Graves-Basedow's disease cases without tumor were characterized via
the round shape (nuclear form factor < 1.15). On the other hand, in
more than 70% of cases where this factor was greater than 1.2, a tumor
was present. Accordingly, if a significant number of the cells are oval
or irregular in shape, other signs of a
potential thyroid tumor must be looked for with great thoroughness. If
other unusual signs are present, the possibility of a tumor must be
considered. In one of our false-negative case, only the oval shape of
the cells and the presence of macrophages could be noted on
hematoxylin-eosin and Giemsa-stained smears at the first cytological
investigation. The original report was benign. 2 years later, when
repeated FNAC was performed and we applied the Papanicolau method for
staining, nuclear grooves could also be observed and the patient was
sent for operation: histopathological examination revealed papillary
cancer.
Papillarization
This phenomenon, which
is not infrequently seen in histopathological slides, occurs only in
rare cases in cytology.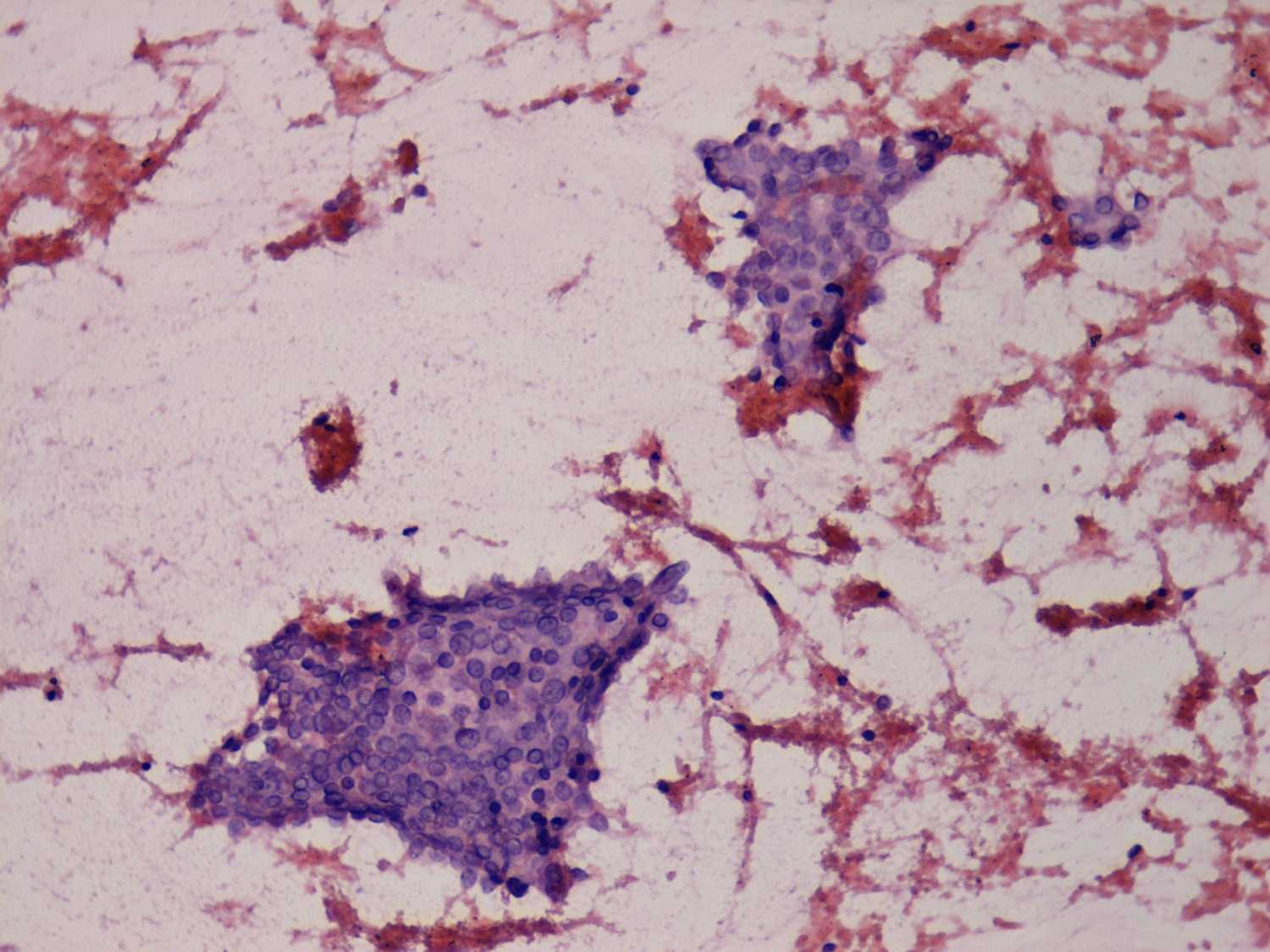 The correct interpretation may be very difficult, because analysis of
the nuclear details is not simple in hyperthyroidism. First, the nuclei
are pale. Moreover, the vacuoles characteristic of Graves-Basedow's
disease may overlap the nuclei and in this case it may be impossible to
detect the typical intranuclear inclusions observed in papillary
cancer. The latter problem stems from the relatively common occurrence
of nuclear grooves in Graves-Basedow's disease. In around half of the
cases where papillarization is present in a smear from a nodule of a
patient with Graves-Basedow's disease, no other feature of papillary
cancer may be observed. In the other half of the cases, the patients
must be sent for operation.
The correct interpretation may be very difficult, because analysis of
the nuclear details is not simple in hyperthyroidism. First, the nuclei
are pale. Moreover, the vacuoles characteristic of Graves-Basedow's
disease may overlap the nuclei and in this case it may be impossible to
detect the typical intranuclear inclusions observed in papillary
cancer. The latter problem stems from the relatively common occurrence
of nuclear grooves in Graves-Basedow's disease. In around half of the
cases where papillarization is present in a smear from a nodule of a
patient with Graves-Basedow's disease, no other feature of papillary
cancer may be observed. In the other half of the cases, the patients
must be sent for operation.
Nuclear grooves are present in the smear
First,
we must rule out the possibility that these grooves are pseudo-grooves.
As mentioned above, the nuclei in Graves-Basedow's disease are pale.
This is a  condition
which favours the border of a cell group or the border of an
overlapping
cell appearing on the light nucleus as a ceased formation. If this
possibility can be ruled out, we cannot exclude the possibility of
papillary cancer, even when no other feature of papillary cancer is
present. We have one more opportunity to avoid a false-positive
diagnosis of papillary cancer, which was the only help in two of our
cases. We performed a repeated aspiration on another part of the
thyroid, and could detect typical grooves in these smears, which
practically excluded the possibility of papillary cancer. We mention
that, in most cases where nuclear grooves were present in smears from
hyperthyroid patients, the signs of underlying lymphocytic thyroiditis
could be detected. On the basis of this observation, if we see numerous
nuclei with grooves, we look for other signs of lymphocytic
thyroiditis.
condition
which favours the border of a cell group or the border of an
overlapping
cell appearing on the light nucleus as a ceased formation. If this
possibility can be ruled out, we cannot exclude the possibility of
papillary cancer, even when no other feature of papillary cancer is
present. We have one more opportunity to avoid a false-positive
diagnosis of papillary cancer, which was the only help in two of our
cases. We performed a repeated aspiration on another part of the
thyroid, and could detect typical grooves in these smears, which
practically excluded the possibility of papillary cancer. We mention
that, in most cases where nuclear grooves were present in smears from
hyperthyroid patients, the signs of underlying lymphocytic thyroiditis
could be detected. On the basis of this observation, if we see numerous
nuclei with grooves, we look for other signs of lymphocytic
thyroiditis.
Numerous lymphocytes in the smear
The distinction between
Graves-Basedow's and Hashimoto's disease is not sharp. This is
particularly true because they represent two clinical forms of the same
entity, autoimmune thyroid disease (AITD). In clinical practice, we can
often observe that typical Hashimoto's thyroiditis evolves in a patient
with Graves-Basedow's disease years or decades after the hyperthyroid
phase. The opposite can also happen, but only infrequently.
On the other hand, from a clinical aspect, the distinction between the
two forms of the AITD has therapeutic consequences in hyperthyroid
patients. FNAC has a particularly important role in those cases where
the serum level of autoantibodies against the TSH receptor is not
elevated (10-15% of the cases), or where this investigation is not
performed. A cytological picture consistent with Hashimoto's
thyroiditis has greater predictive value than one consistent with
Graves-Basedow's disease. (Lymphocytic thyroiditis may present in
multifocal form, and therefore may be missed by FNAC.) The presence of
oxyphilic cells without lymphocytes does not decide the question ( Orell
1997 ). Moreover, a small number of lymphocytes can be detected
in most smears of typical Graves-Basedow's disease. The presence of
nuclear debris favours the diagnosis of Hashimoto's thyroiditis ( Droese
1987 ). Hence, a clear distinction is not possible in a
relatively high number of cases. For our results, see TABLE
Therapy-related changes in patients previously treated for hyperthyroidism
Thyrostatic drugs
aggravate the cellular atypia characteristic of hyperthyroidism. Si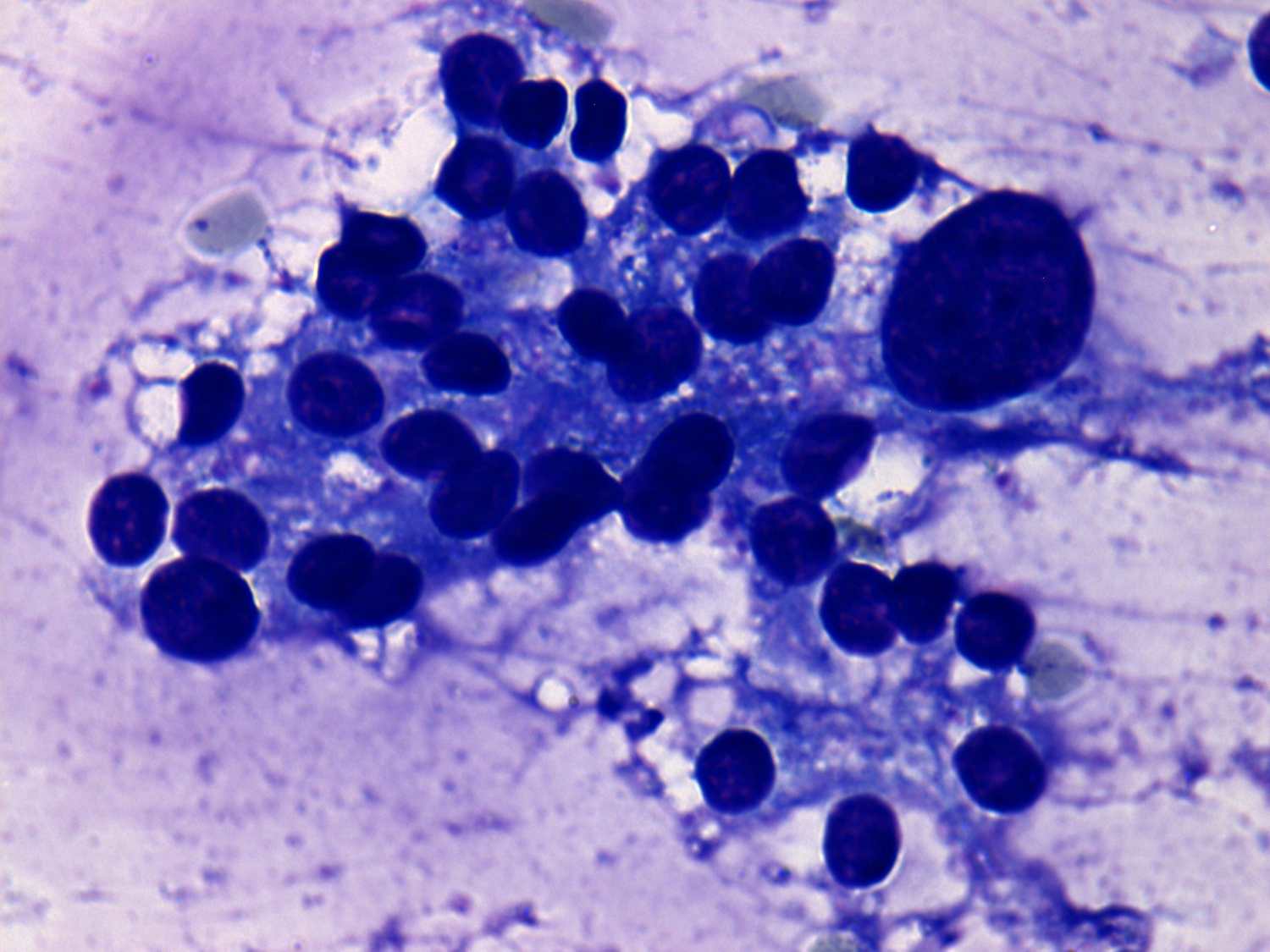 ngle, highly-enlarged, hyperchromatic,
but round cells relatively often occur in the smear. We have
only exceptionally observed change in the form of well-preserved
thyrocytes. On the other hand, it must be borne in mind that the
changes caused by a thyrostatic drug can be observed decades after the
therapy, irrespective of the actual hormonal state of the patient.
ngle, highly-enlarged, hyperchromatic,
but round cells relatively often occur in the smear. We have
only exceptionally observed change in the form of well-preserved
thyrocytes. On the other hand, it must be borne in mind that the
changes caused by a thyrostatic drug can be observed decades after the
therapy, irrespective of the actual hormonal state of the patient.
Patients
who have received a previous isotope therapy for hyperthyroidism rarely
need FNAC. In such cases, we have observed pronounced degenerative
changes. Beside enlargement of the cell, polymorphis m can also
be seen (Granter 1997). However, most of these highly
polymorphic cells are degenerated. In these cases, awareness of the
previous radioactive iodine treatment is particularly important for the
cytopathologist to avoid overdiagnosis of the cytological picture (Centeno
1996, Granter 1997).
m can also
be seen (Granter 1997). However, most of these highly
polymorphic cells are degenerated. In these cases, awareness of the
previous radioactive iodine treatment is particularly important for the
cytopathologist to avoid overdiagnosis of the cytological picture (Centeno
1996, Granter 1997).
