Intranodular hyperechogenic figures - case 1137 |
|
First investigation
Clinical presentation: A 37-year-old hypothyroid woman was referred for an evaluation of neck discomfort and fever. She lost 5 kg in weight and had palpitation. Her complaints lasted for 3 weeks.
Palpation: The thyroid was moderately firm.
Results of blood test: mild hyperthyroidism with TSH 0.05 mIU/L, FT4 30.1 pM/L, FT3 8.99 pM/L, aTPO 2 U/mL, TSAb negative, erythrocyte sedimentation rate 31 mm/H, CRP 8,9 mg/L (normal value: 0-4.8).
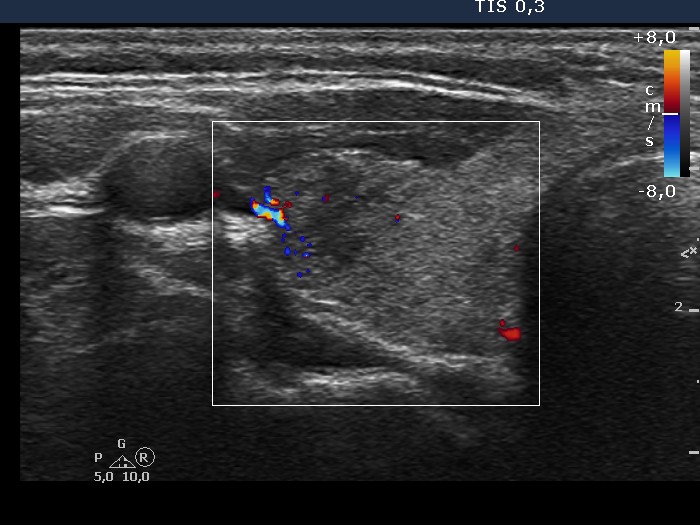
Ultrasonography: The thyroid was minimally hypoechogenic and contained multiple small hypoechogenic areas with sharp, puzzle-like borders. The vascularization was a little bit increased.
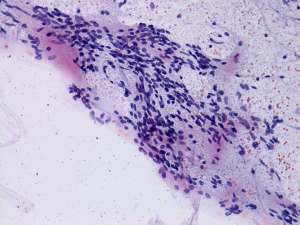
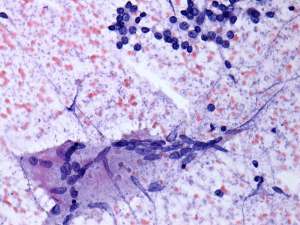
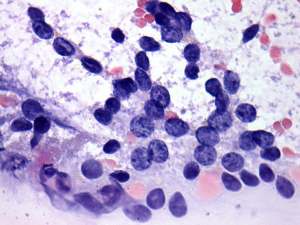
Cytology: The largest hypoechogenic lesion in the ventromedial part of the left lobe was aspirated. The cytological pattern was consistent with thyroiditis.
Combined clinical-sonographic-cytological diagnosis: Hashimoto's thyroiditis with hashitoxicosis.
We administered beta blocking agent and non-steroid anti-inflammatory drug.Results of follow-up.
6 weeks later the patient became hypothyroid (TSH 11.7 mIU/L, FT4 8.09 pM/L). We gave no replacement therapy. The patient did not use the NSAID because her neck complaints resolved the next day after the examination and did not recur later.
6 months later the hypothyroidism has worsened (TSH 38.7 mIU/L, FT4 < 6 pM/L) while aTPO resulted in 728 U/ml, erythrocyte sedimentation rate and CPR were in the normal range.
Comments.
-
Three possibilities had to be considered: Graves' disease, de Quervain's thyroiditis and Hashimoto's thyroiditis. Although the clinical data and blood tests favored de Quervain's thyroiditis, moreover the cytological pattern was consistent with this possibility, the sonographic pattern practically excluded this disease because the hypoechogenic areas were sharp and have puzzle-like borders and the vascularization was increased.
-
Multinucleated giant cells occur rarely in Hashimoto's thyroiditis, while the pattern with multinucleated areas composed of epithelioid cells is an even more rare phenomenon.
-
The normal antibody levels argued against the possibility of autoimmune thyroid disease, but by no way excluded this possibility. The elevated ESR and CRP levels and the neck complaints disclosed clinically subacute disease and were consistent with active state of autoimmune thyroiditis.
-
The follow-up results proved that our original diagnosis was correct. Nevertheless, the possibility that the patient had de Quervain's thyroiditis, too, cannot be excluded.