Subacute granulomatous de Quervain's thyroiditis - Case 43. |
|
First examination (1st to 3rd rows of images):
Clinical presentation: a 47-year-old man was referred for evaluation of complaints suggesting subacute thyroiditis. He suffered from recurrent attacks of pain in the region of the thyroid radiating to the jaws. The pain was originally located to the left side of the neck but for 2 weeks both sides of the neck were affected. He had subfebrility, occasionally fever. He get 3 courses of antibiotics without any effect. The GP initiated investigation toward lymphoma of the neck.
Palpation: both thyroids were hard and painful.
Laboratory tests: euthyroidism with TSH-level 0.27 mIU/L, FT4 16.7 pM/L, CRP 35.1 mg/L, ESR 41 mm/H, aTPO 10 U/mL.
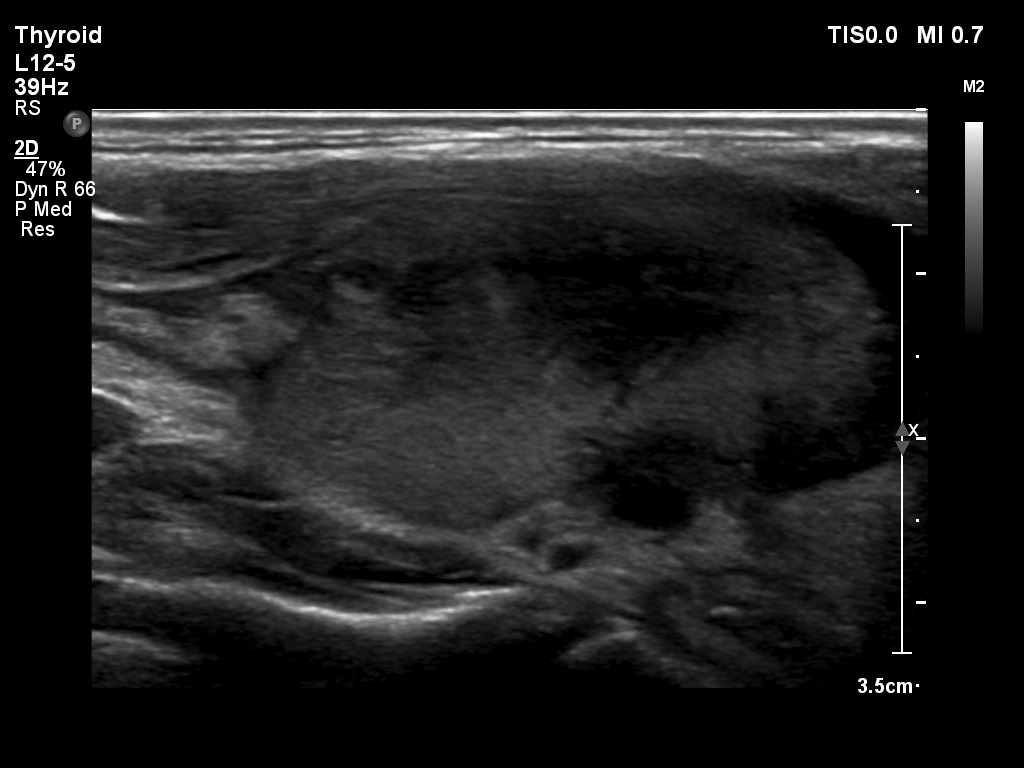
Ultrasonography: both lobes presented hypoechogenic ill-defined areas. The echogenicity index was 80% in the right lobe while 20% in the left thyroid. The vascularization was significantly decreased.
Elastography demonstrated hard areas according to the hypoechogenic field in the left lobe while almost the entire right lobe proved to be hard.Cytological diagnosis: subacute, granulomatous de Quervain's thyroiditis.
Suggestion: steroid therapy was initiated and resulted in prompt amelioration of complaints.
Intermediate consultation 3 month after initial examination:
Clinical state: the complaints of the patients ceased within a day after steroid therapy and did not recur even after discontinuation of the 6-week steroid therapy. His blood pressure temporarily increased while on steroid therapy but normalized without medical intervention.
Laboratory tests: euthyroidism with TSH-level 21.3 mIU/L, FT4 8.3 pM/L, CRP 1.6 mg/L.
We suggested the next checking of thyroid function in 6 months.
Second examination 14 months after the initial (4th row of images):
Clinical examination: the patient had no complaints.
Palpation: the thyroid was not palpable.
Ultrasonography: the size of the thyroid decreased dramatically and became atrophic. The right lobe already presented a small severely hypoechogenic area. In contrast with the first examination the basic echo structure of the left lobe was not normal but moderately hypoechogenic. The vascularization was decreased and average, right and left lobe, respectively.
Laboratory tests: hypothyroidism with TSH-level 13.8 mIU/L, FT4 11.4 pM/L, CRP 1.1 mg/L, aTPO 9 U/mL.
Suggestion: considering the improving the TSH we suggested repeat blood test in 6 months but did not start with replacement therapy.
Comments.
-
There were several unusual findings in this patient. First, the thyroids contained severely hypoechogenic areas and the borders of the hypoechogenic areas were rather puzzle-like than ill-defined. The latter increased the possibility of a concomitant autoimmune thyroiditis.
-
Nevertheless, the patient had not only clinically but even cytologically subacute thyroiditis at first examination; the cytology is decisive.
-
More than 95% of patients with subacute thyroiditis present a complete normalization of thyroid functions one year after the last painful episode while the TSH of this patient remained elevated 14 months after the painful attack. Moreover, the echo pattern of the thyroid remained abnormal, moreover the basic echo structure of the left thyroid worsened, it became hypoechogenic.
-
The case study has not ended. We think that the chance of a permanent hypothyroidism is great primarily not because of the elevated TSH at 14-months examination but because of the ultrasound presentation. There are two possibilities. First, the harm caused by the thyroiditis was more severe and the thyroid requires more time to the complete normalization. Second, the patient have an autoimmune thyroiditis, as well which is responsible of the abnormal ultrasound and TSH finding at the time when the de Quervain's thyroiditis has already healed.
- When we get new data, we will go on doing the case study.
.