Subacute granulomatous de Quervain's thyroiditis - Case 35. |
|
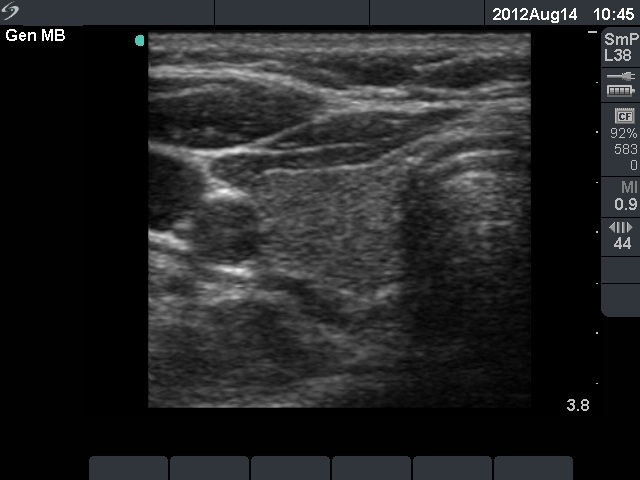
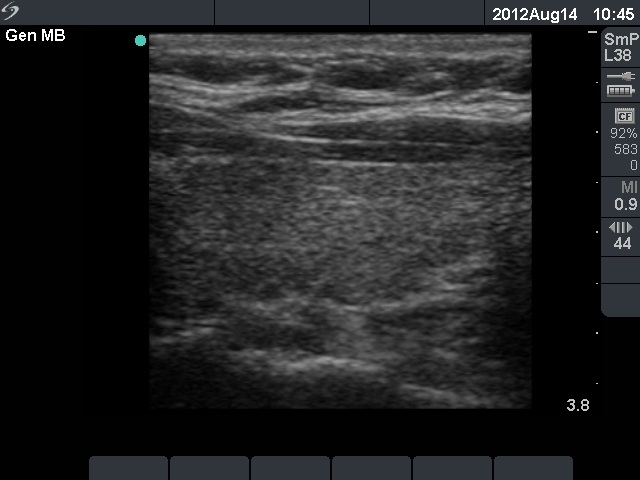
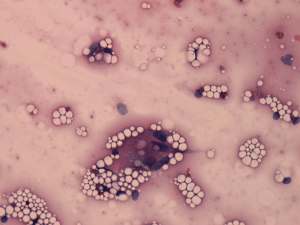
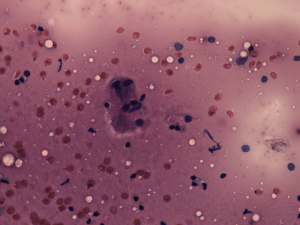
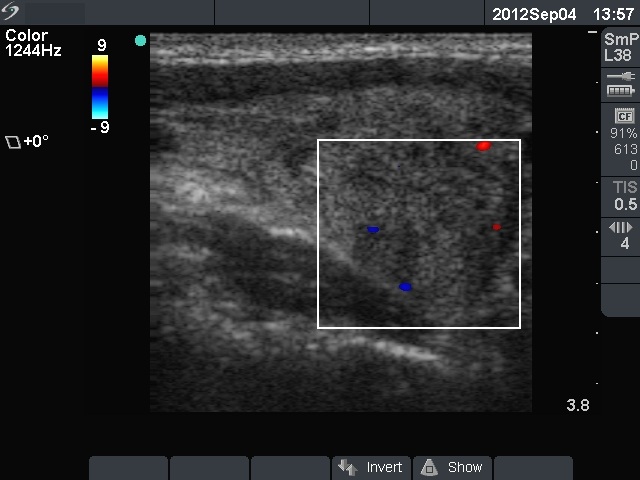
First examination (1st and 2nd rows of images):
Clinical presentation: a 45-year-old woman was referred with typical complaints of subacute thyroiditis: fever, pain in the region of the left thyroid lasting for 4 weeks.
Palpation: the left thyroid was hard and painful, while the right thyroid was moderately firm and not tender.
Functional state: moderate degree of hyperthyroidism with TSH-level 0.001 mIU/L, FT4 35.1 pM/L. ESR 70 mm/H, CRP 21.7 mg/L.
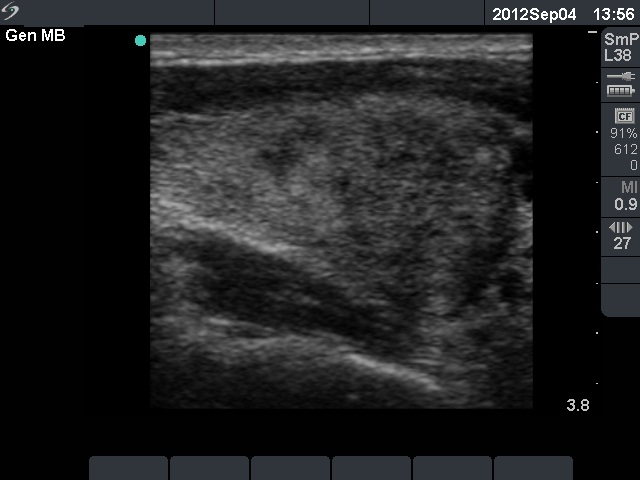
Ultrasonography: there were multiple hypoechogenic areas with blurred borders within echonormal background in the left thyroid. The vascularization was decreased. The right thyroid was intact and had normal vascularization.
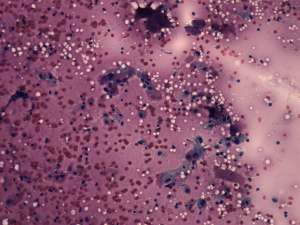
Cytological diagnosis: subacute, granulomatous de Quervain's thyroiditis.
Suggestion: steroid therapy. The complaints of the patient suddenly stopped within 24 hours after the steroid intake.
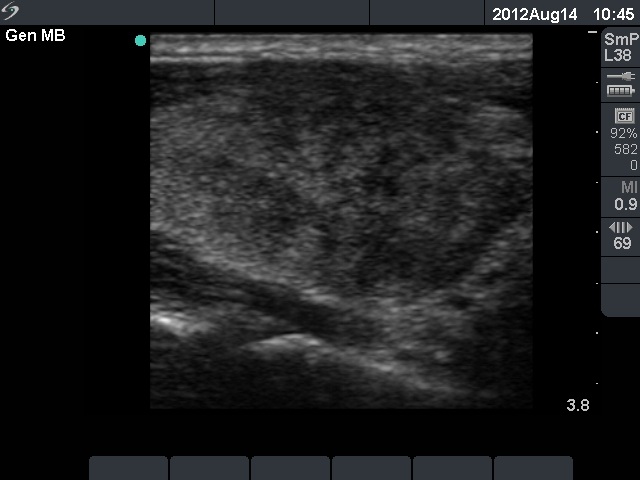
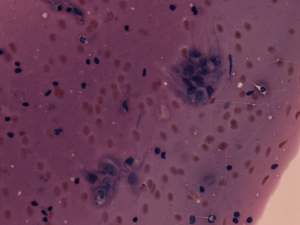
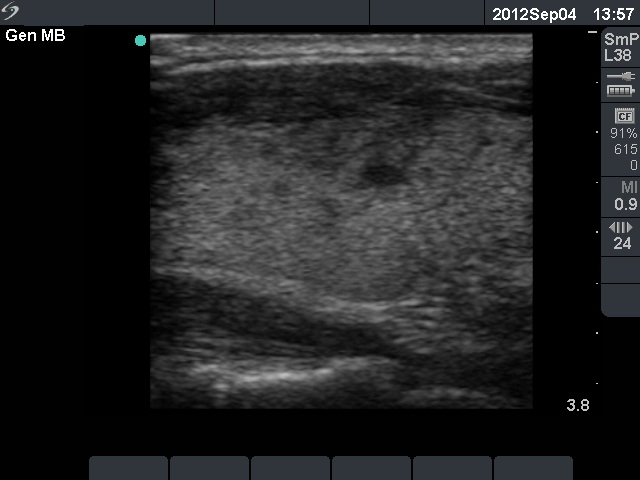
Follow-up examination 3 weeks later (3rd row of images):
Clinical presentation: the patient visited us again because of side effects of steroid - his blood pressure increased significantly. Otherwise she had no complaints.
Palpation: both thyroids were moderately firm but were not tender on palpation.
Functional state: subclinical hyperthyroidism with TSH-level 0.001 mIU/L, FT4 15.1 pM/L. ESR 28 mm/H, CRP 3.7 mg/L.
Ultrasonography: a relatively large hypoechogenic lesion with decreased vascularization has evolved in the previously intact right lobe. On the other hand, the hypoechogenic area in the left lobe significantly decreased in size and the vascularization normalized.