|
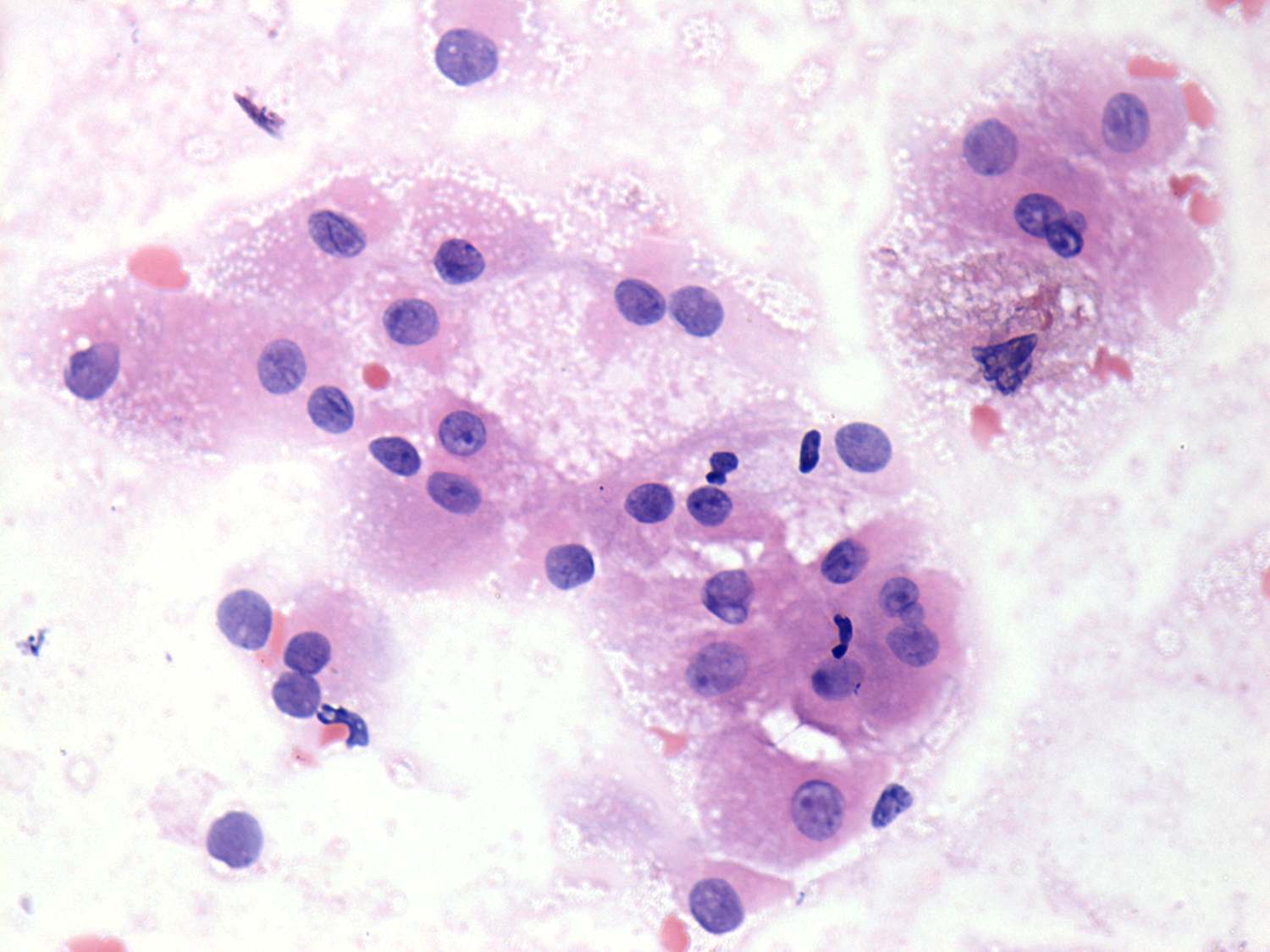
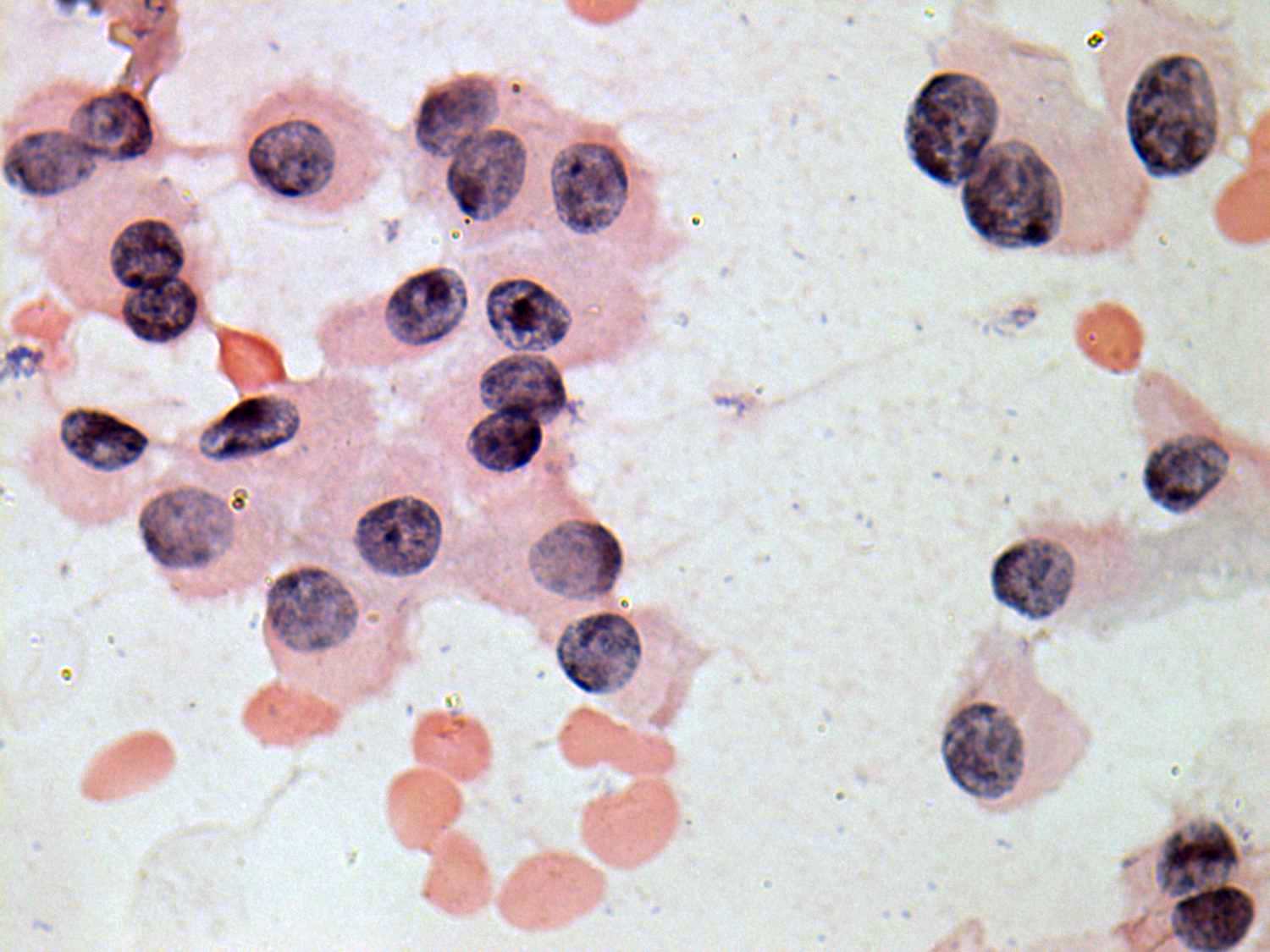
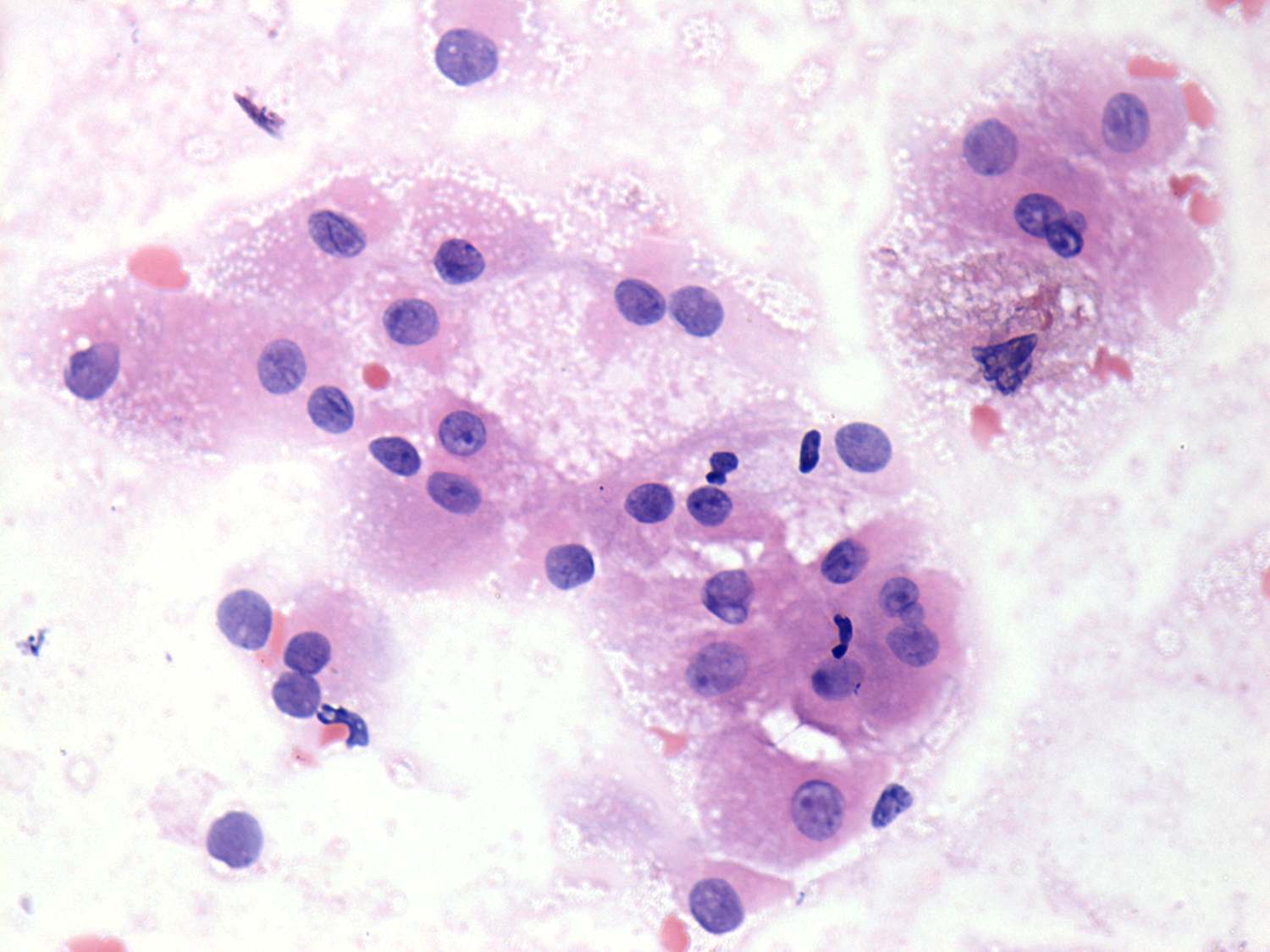
Benign hyperplastic nodule
|
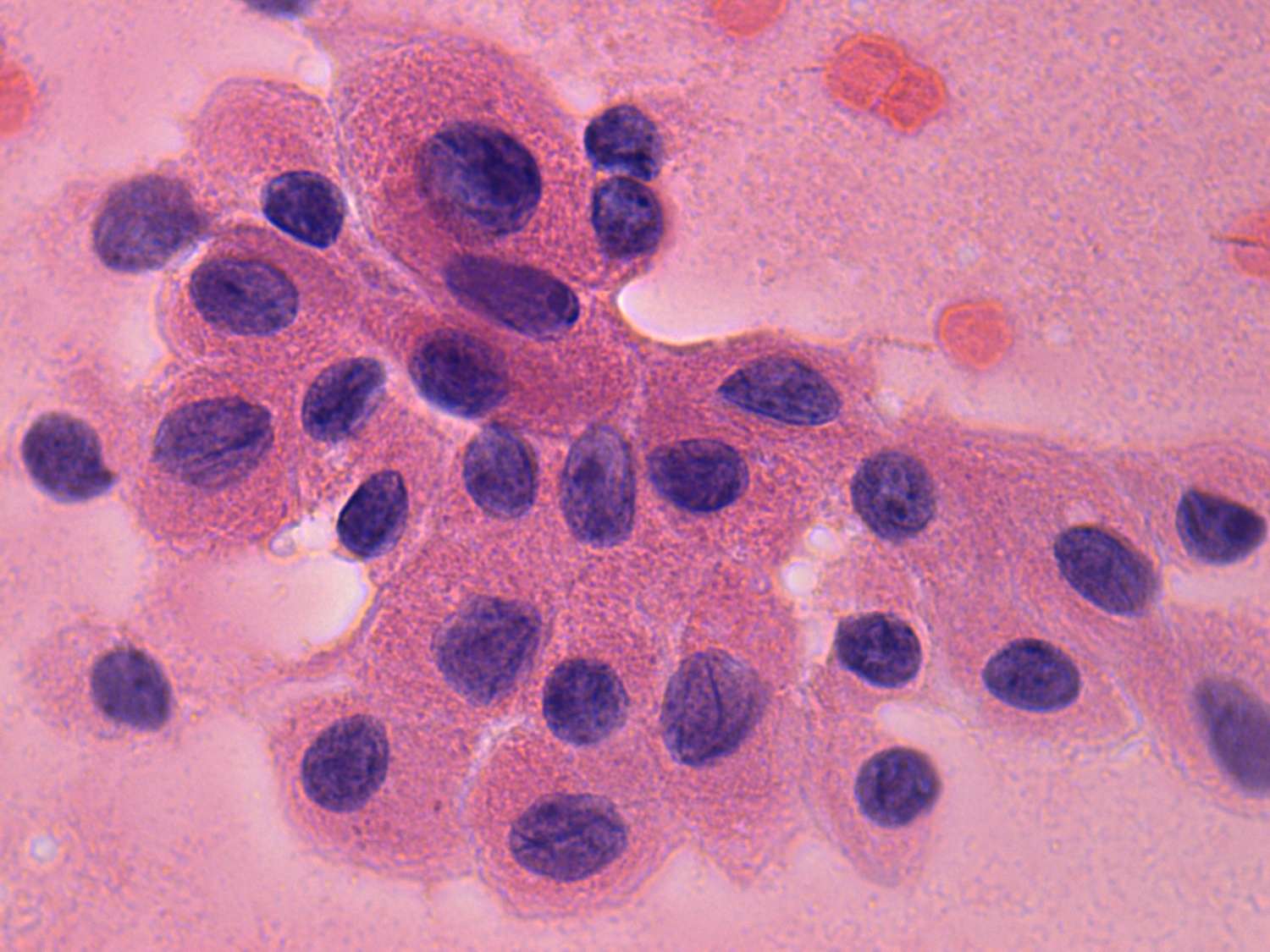
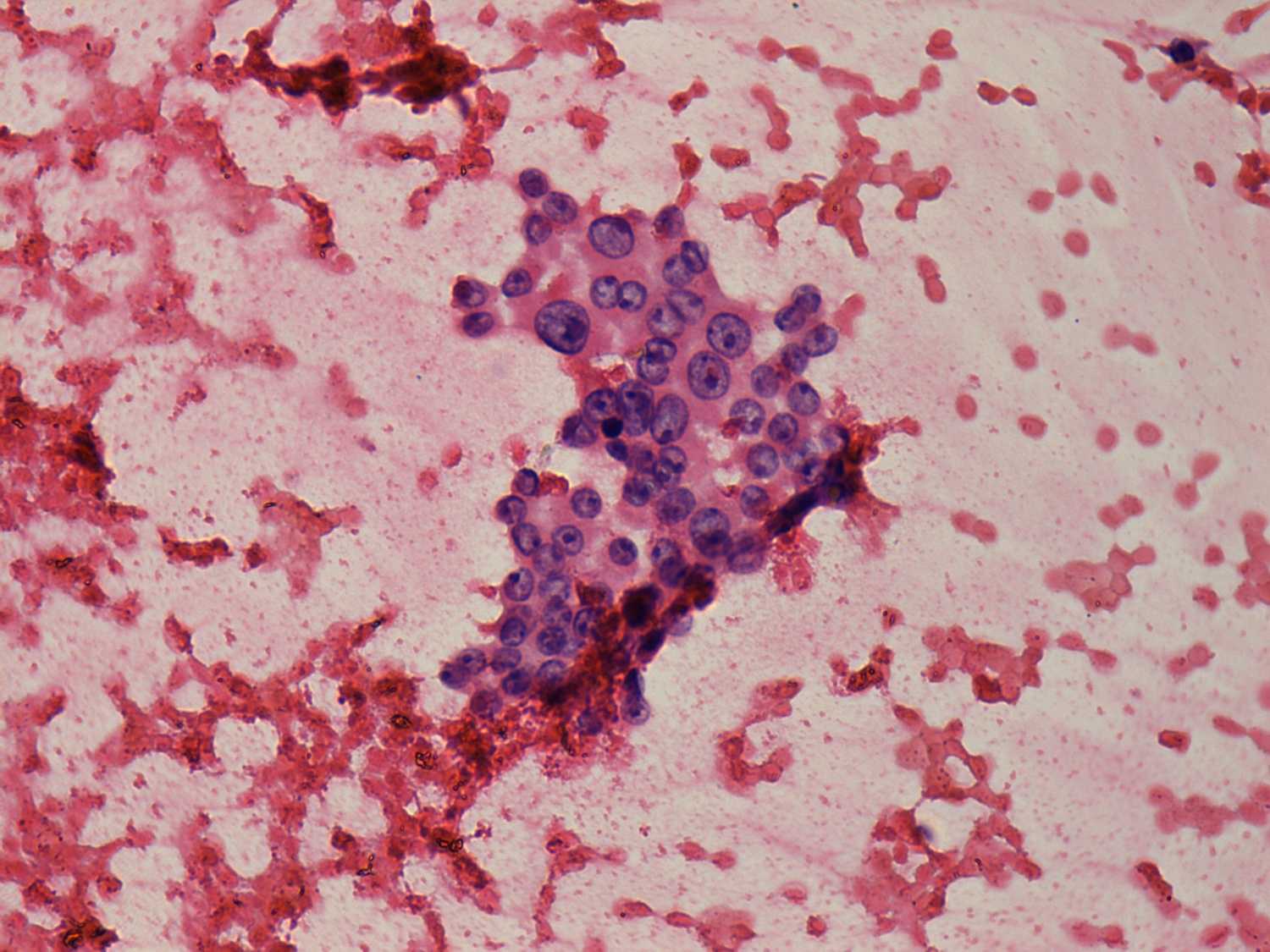
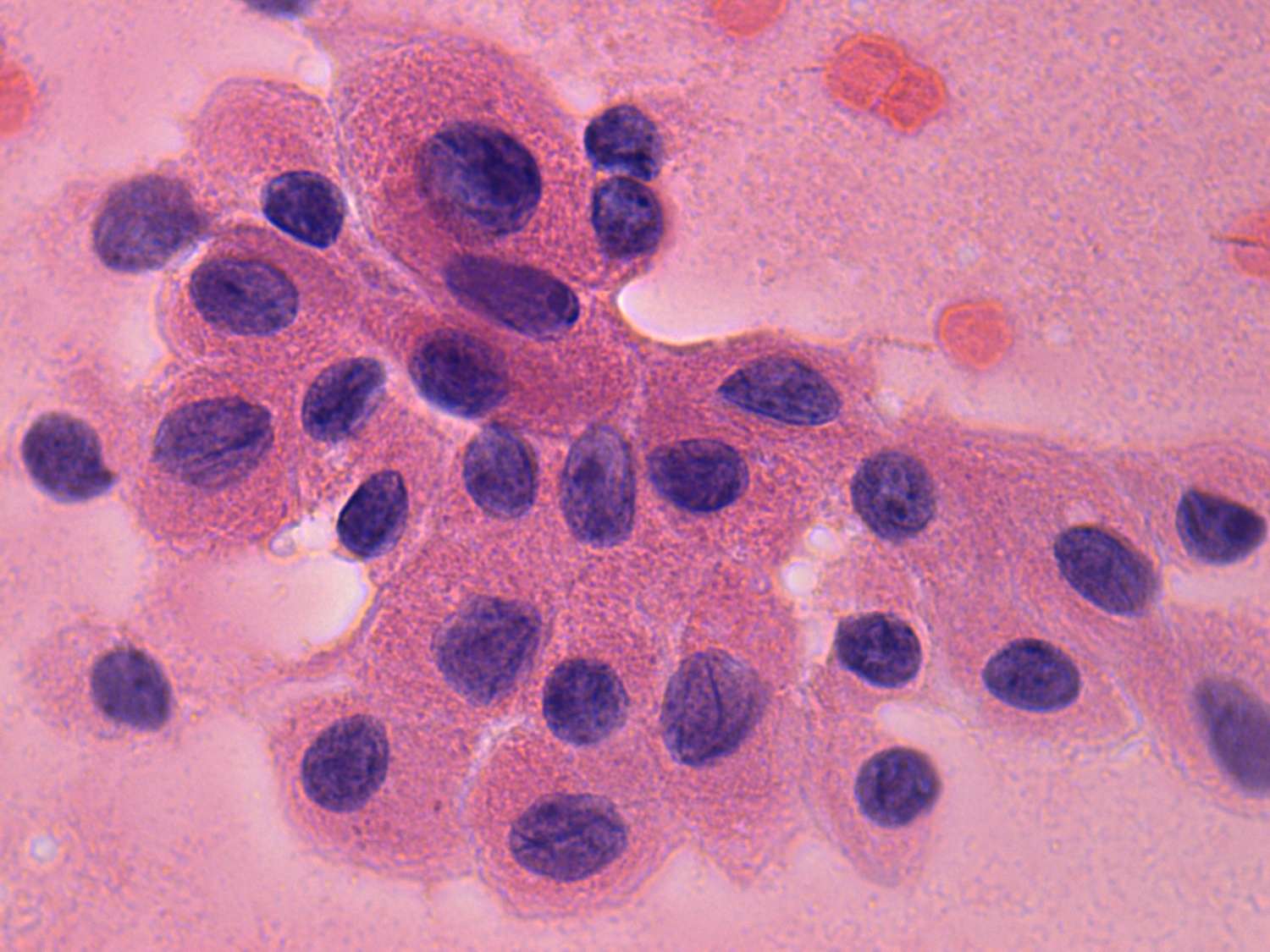
Oxyphilic cancer
|
 |
 |
 |
 |
|
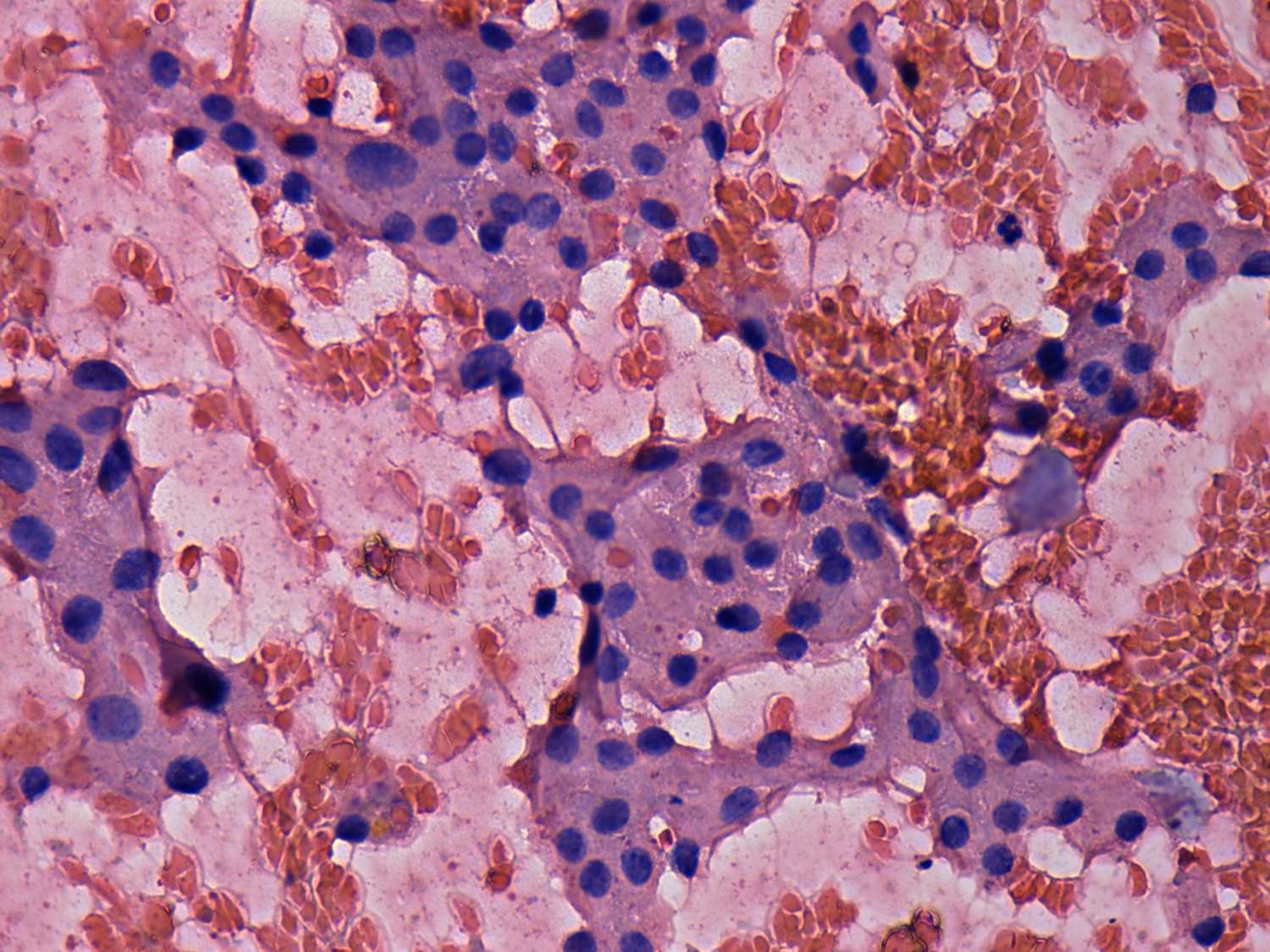
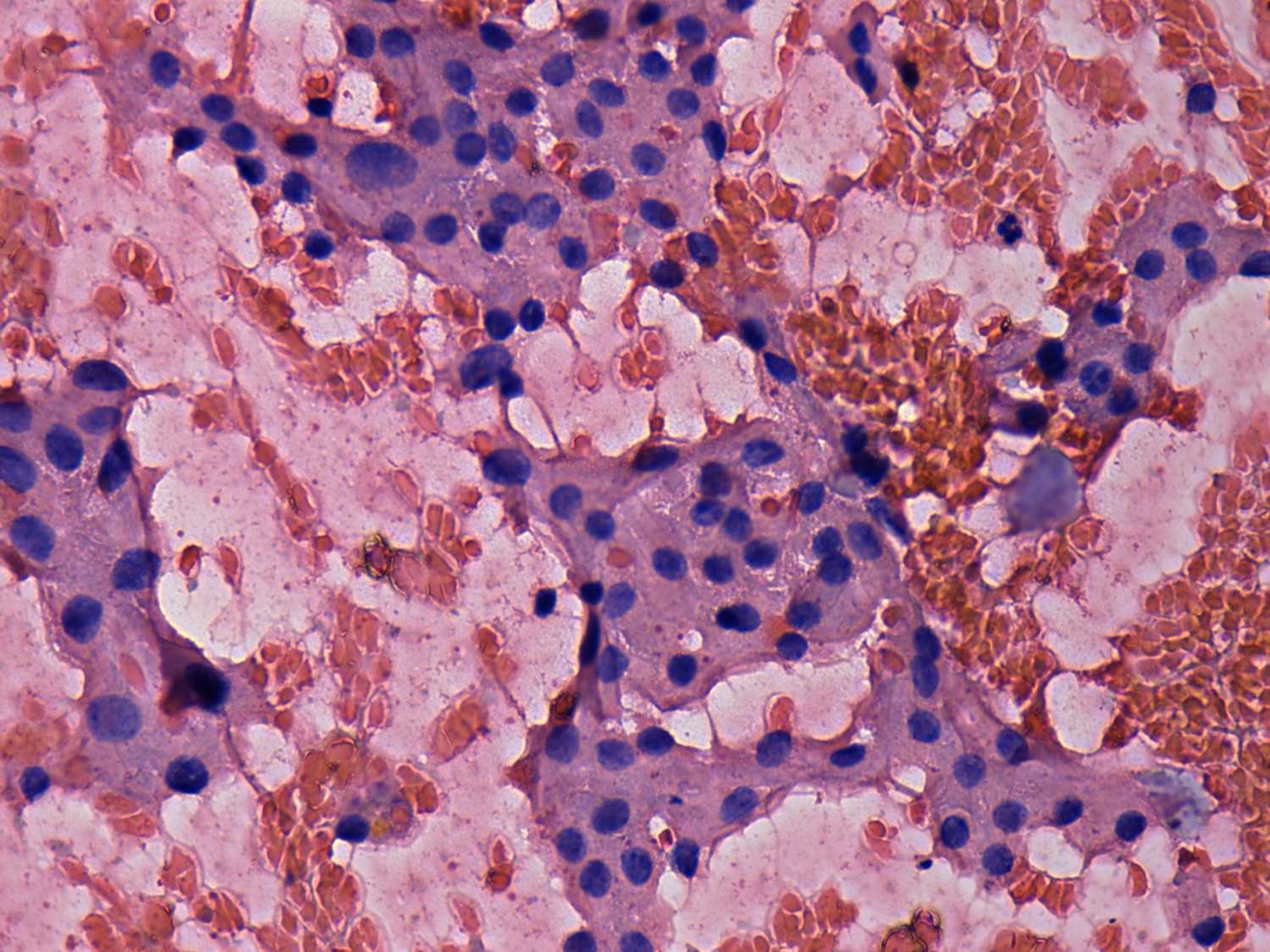
Cohesive groups of oxyhilic cells can be seen. Only a few dissociated
cells can be found. The chromatine structure is blunt. Moreover,
diffuse colloid precipitate can observed.
The risk if a lesion is an oxyphilic tumor is less than 10%
.
|
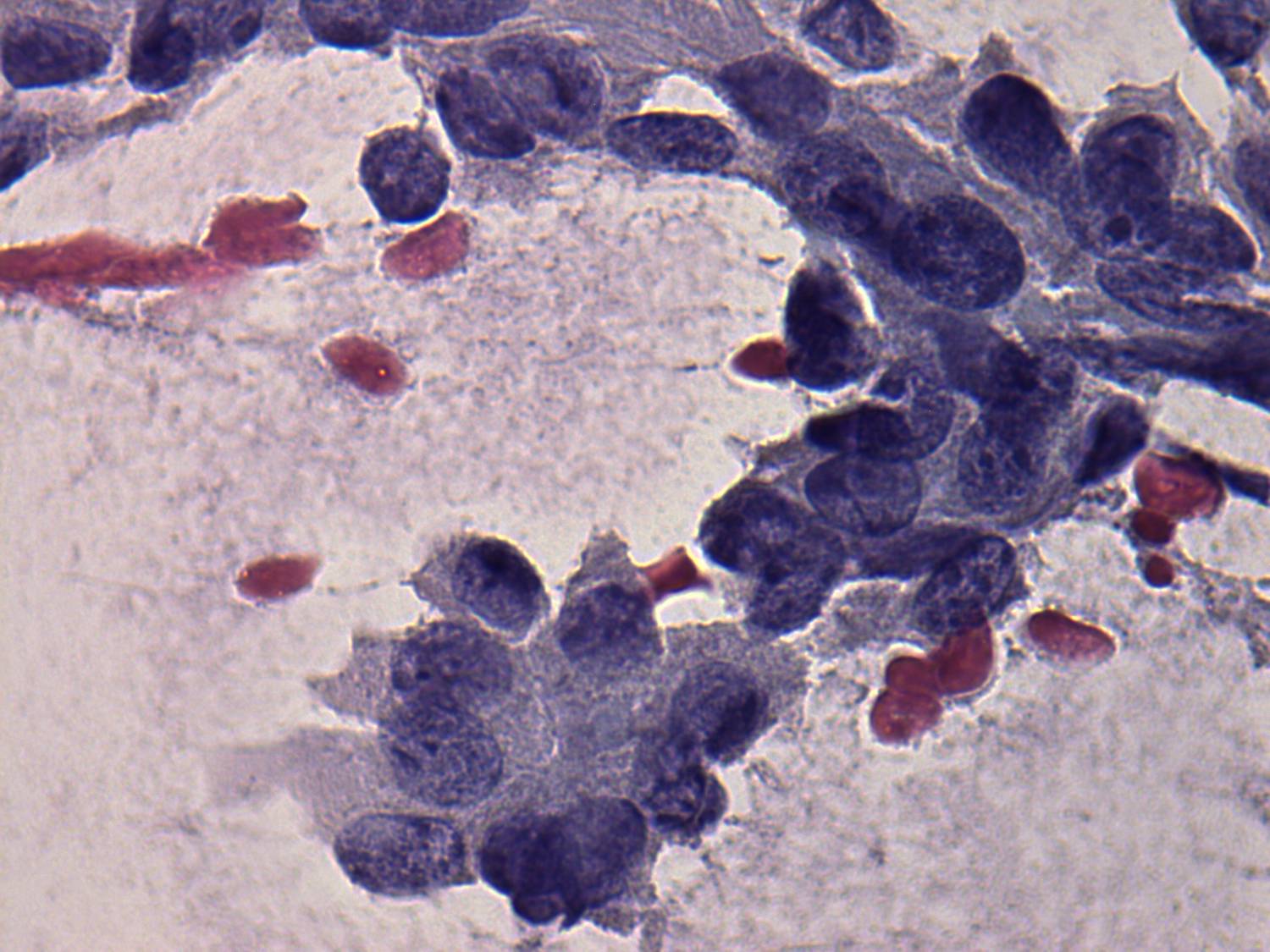
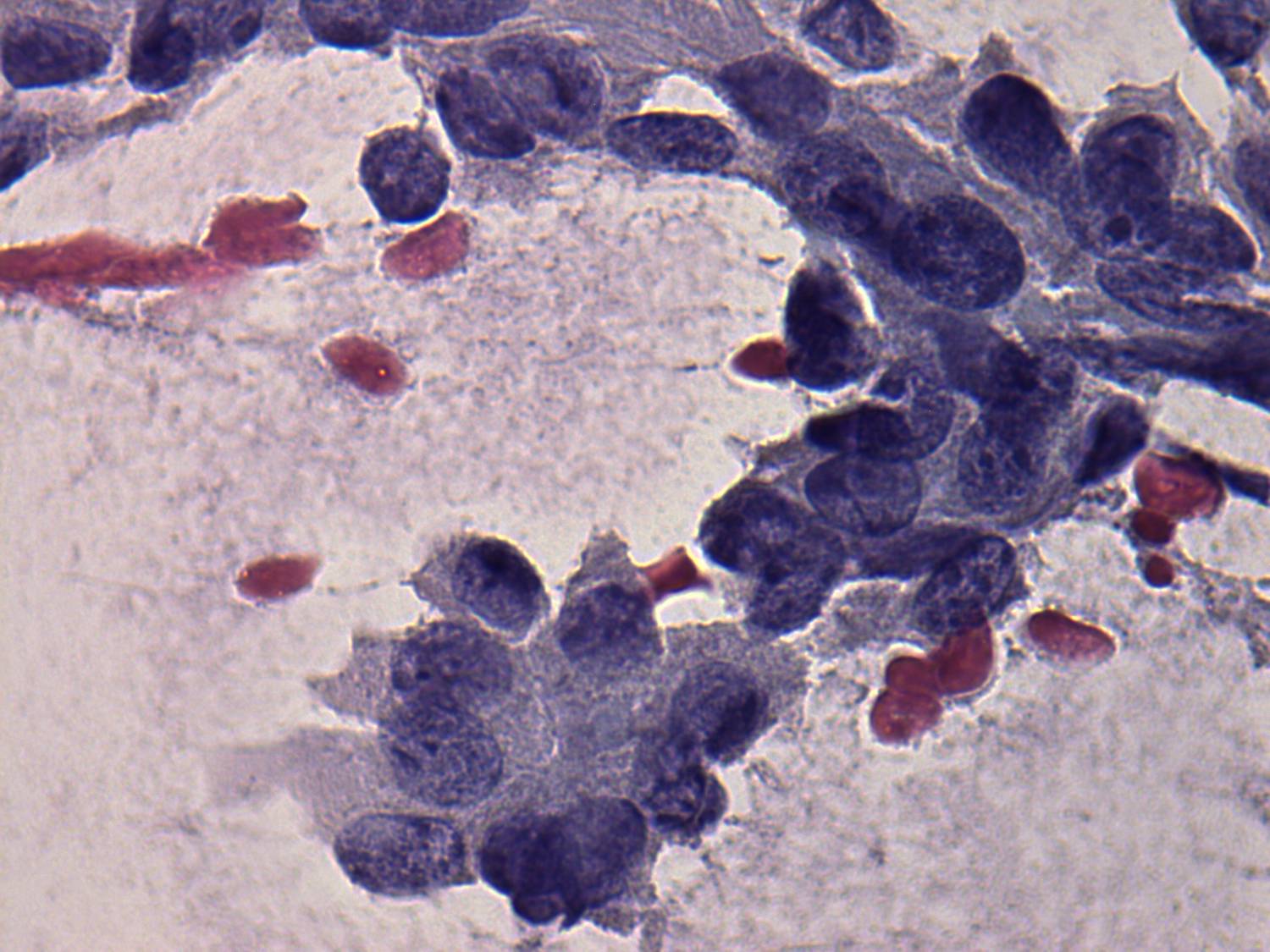
Although oxyphilic cells do not present large prominent nucleoli, they
tend to dissociate. The latter property counts more than the former.
The risk of oxyphilic tumor is more than 50%. |
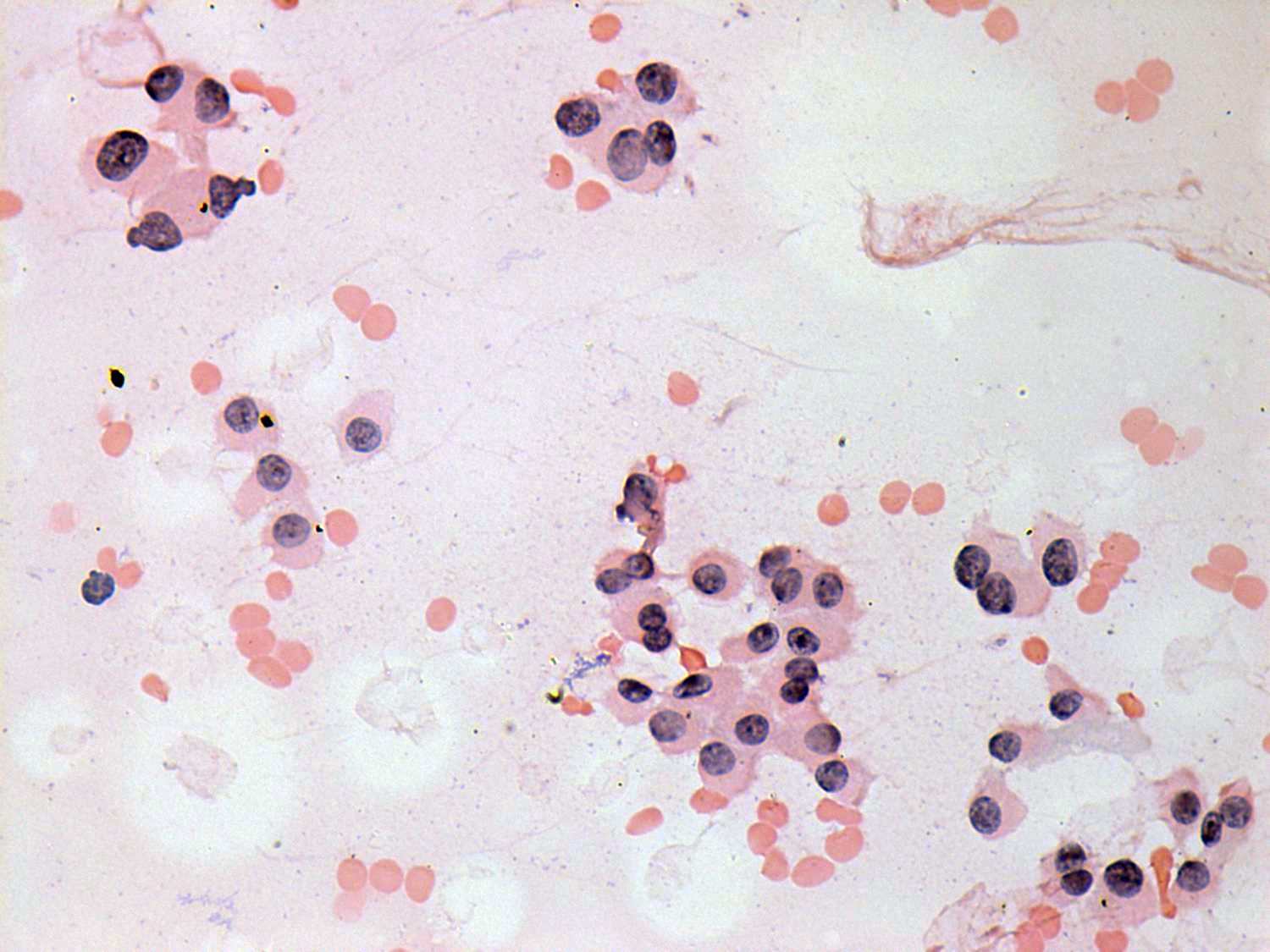
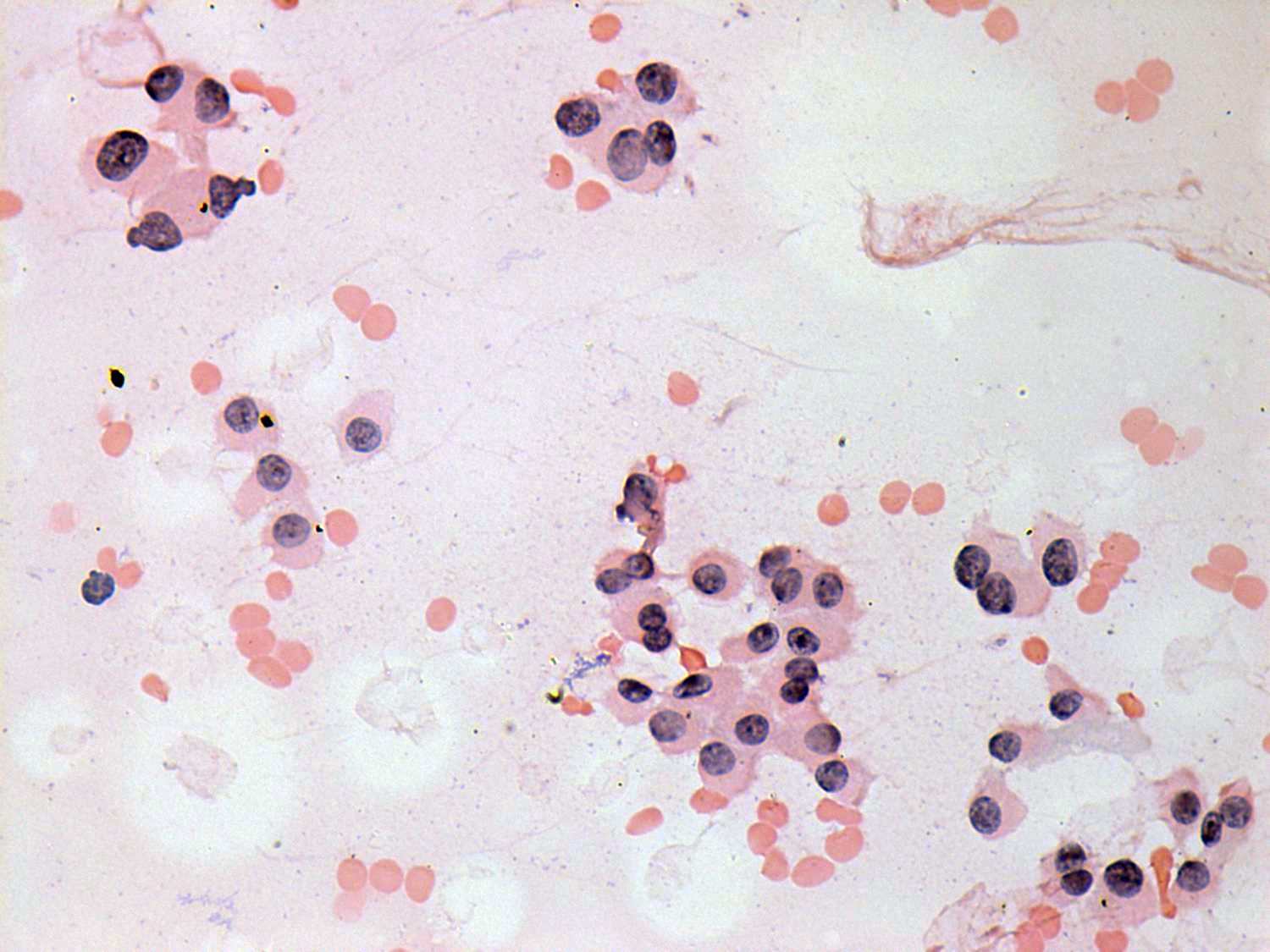
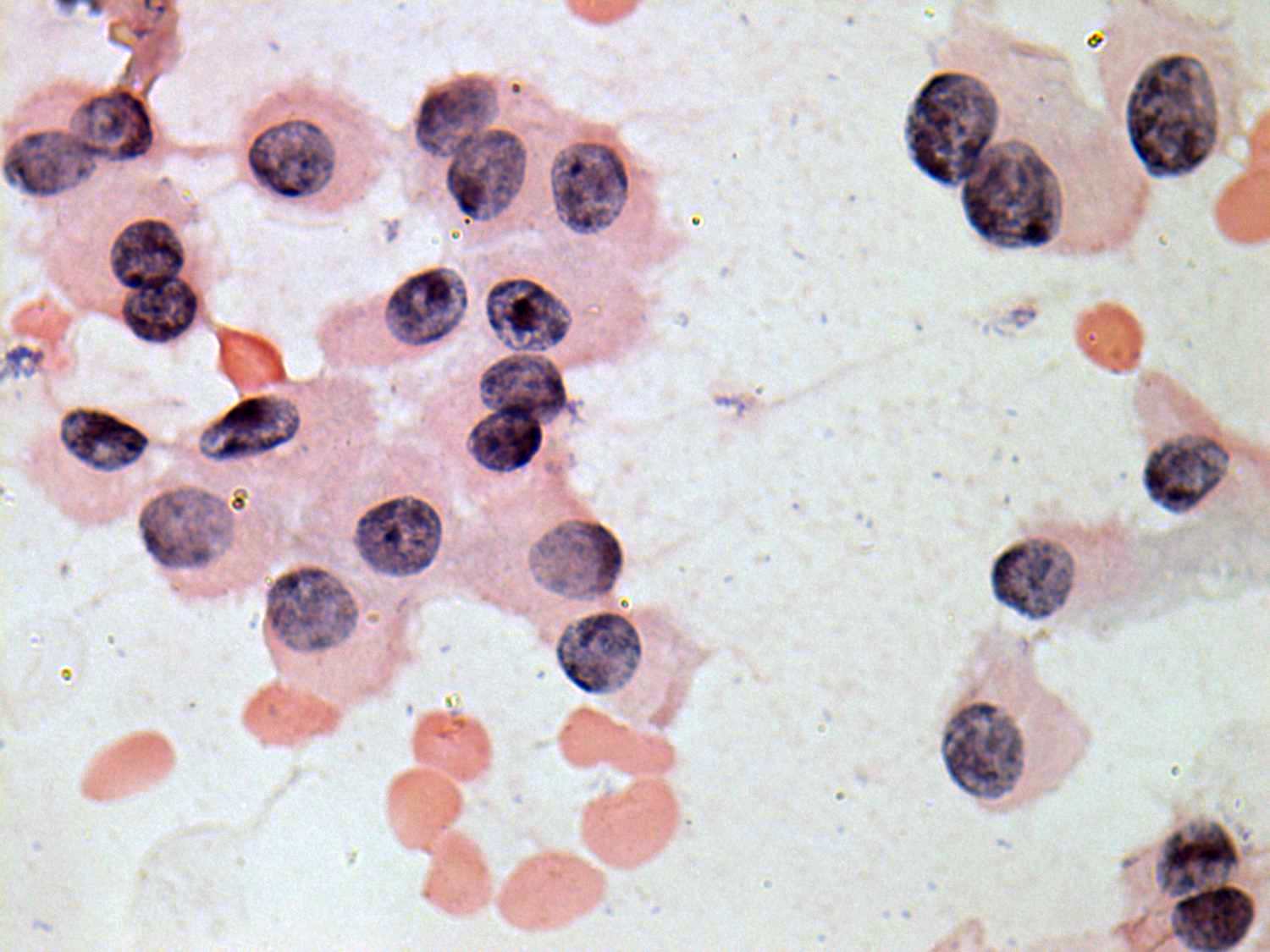
Benign hyperplastic nodule - Case
29 |
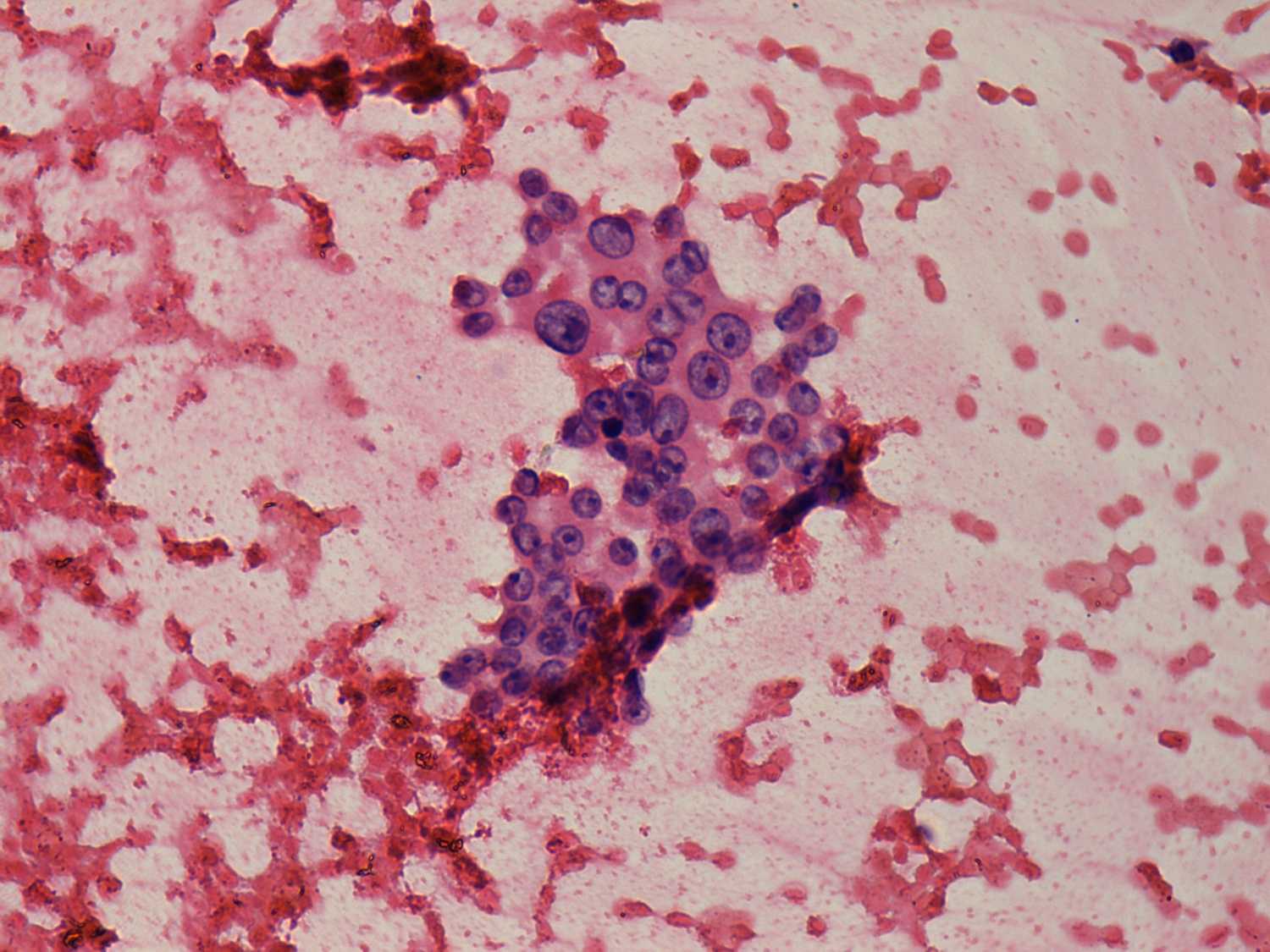
Oxyphilic variant of papillary cancer - Case 70 |
 |
 |
 |
 |
|
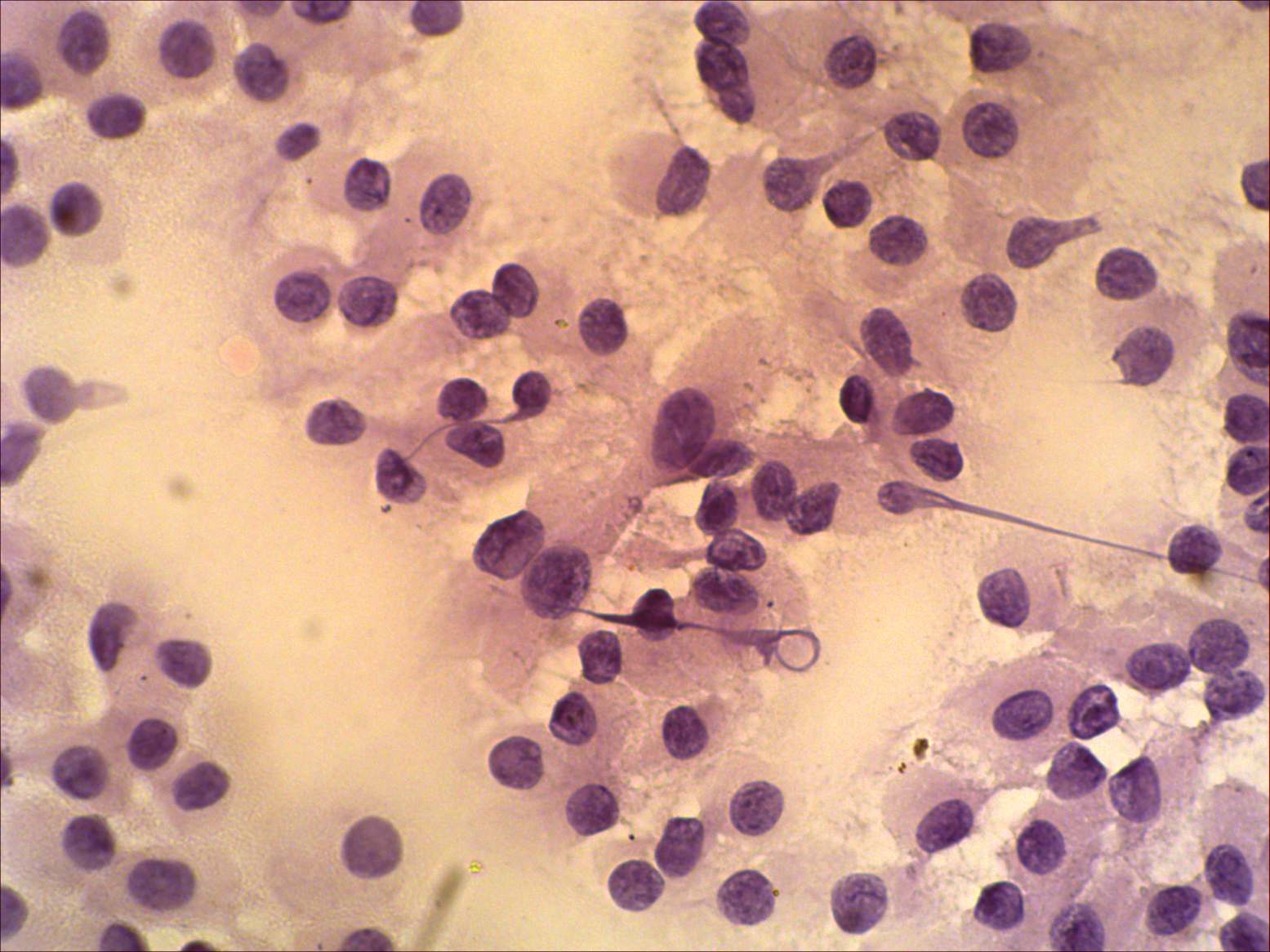
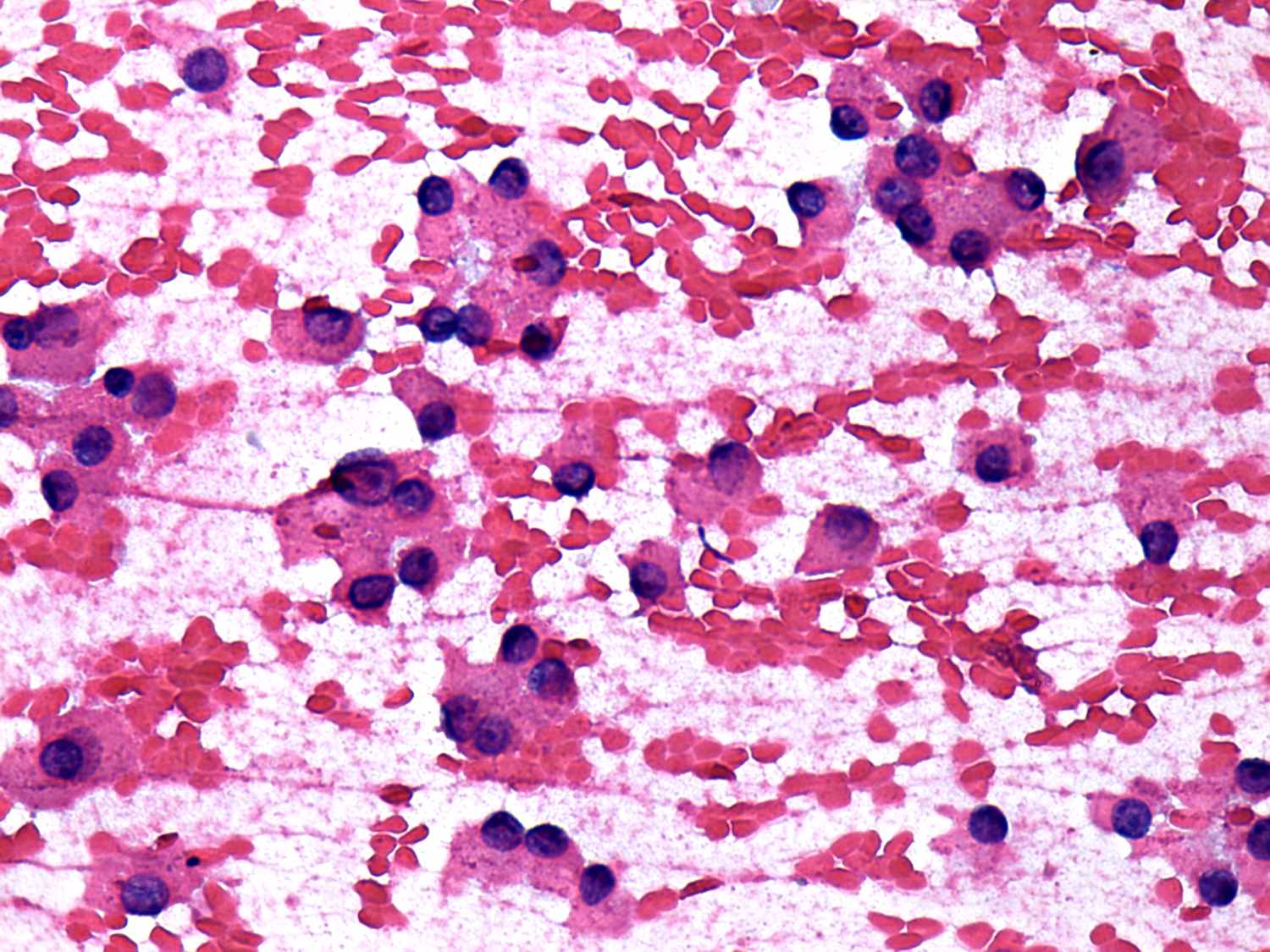
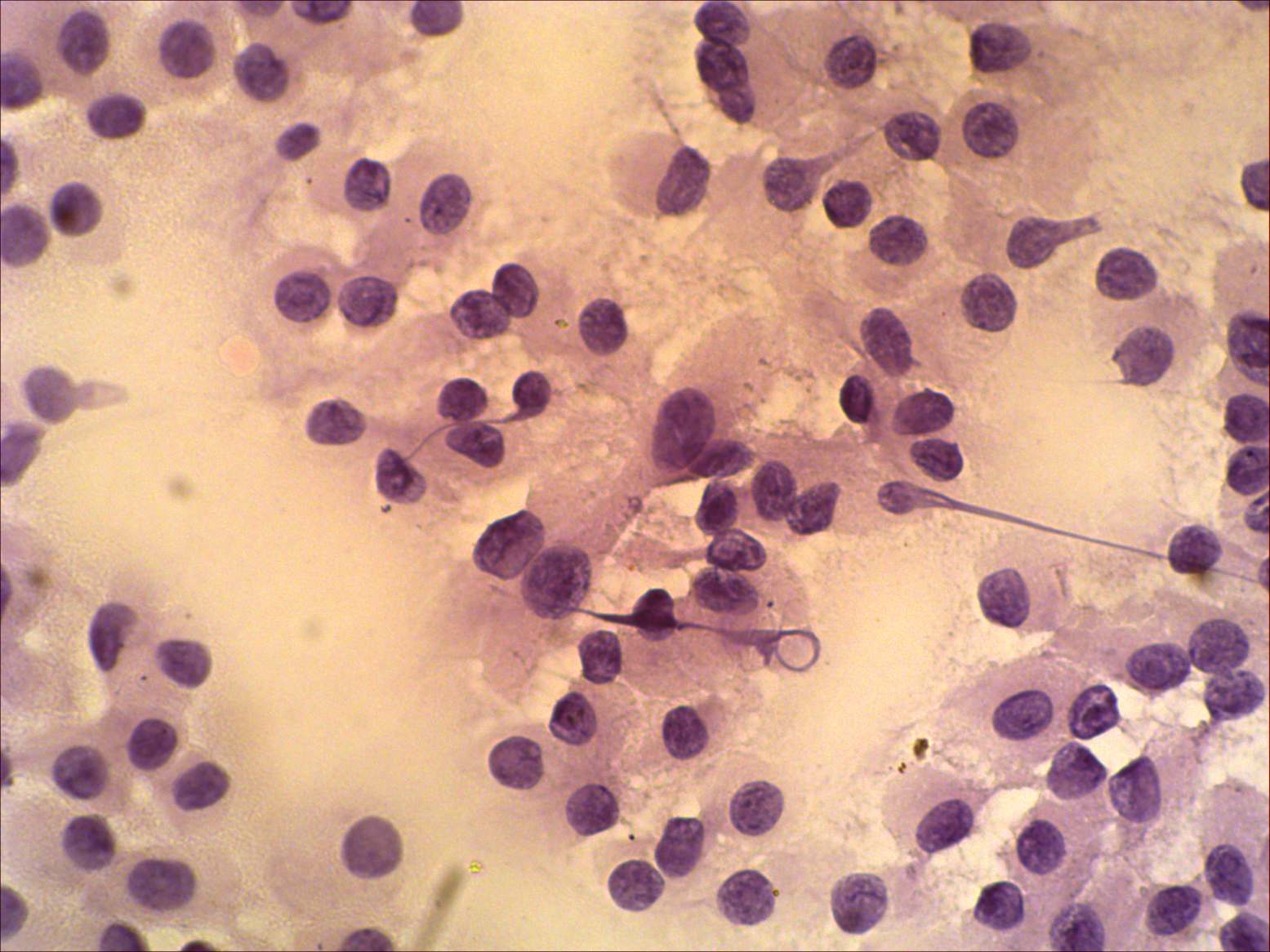
The patterns are very similar. The only difference is in the tendency
of cells to dissociate. This is only limited in the case of
hyperplastic nodule while more pronounced in the case of oxyphilic
adenoma.
|
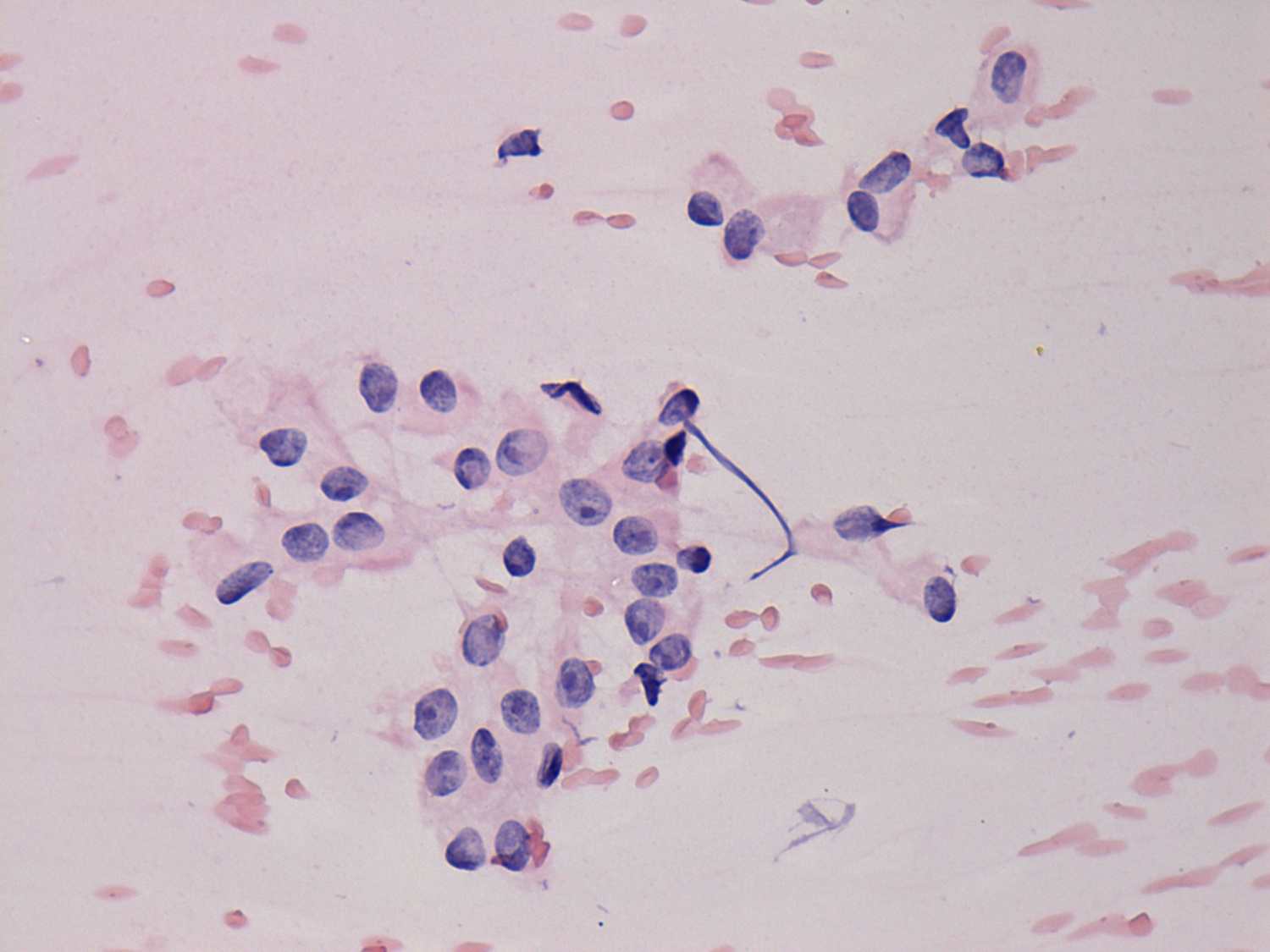
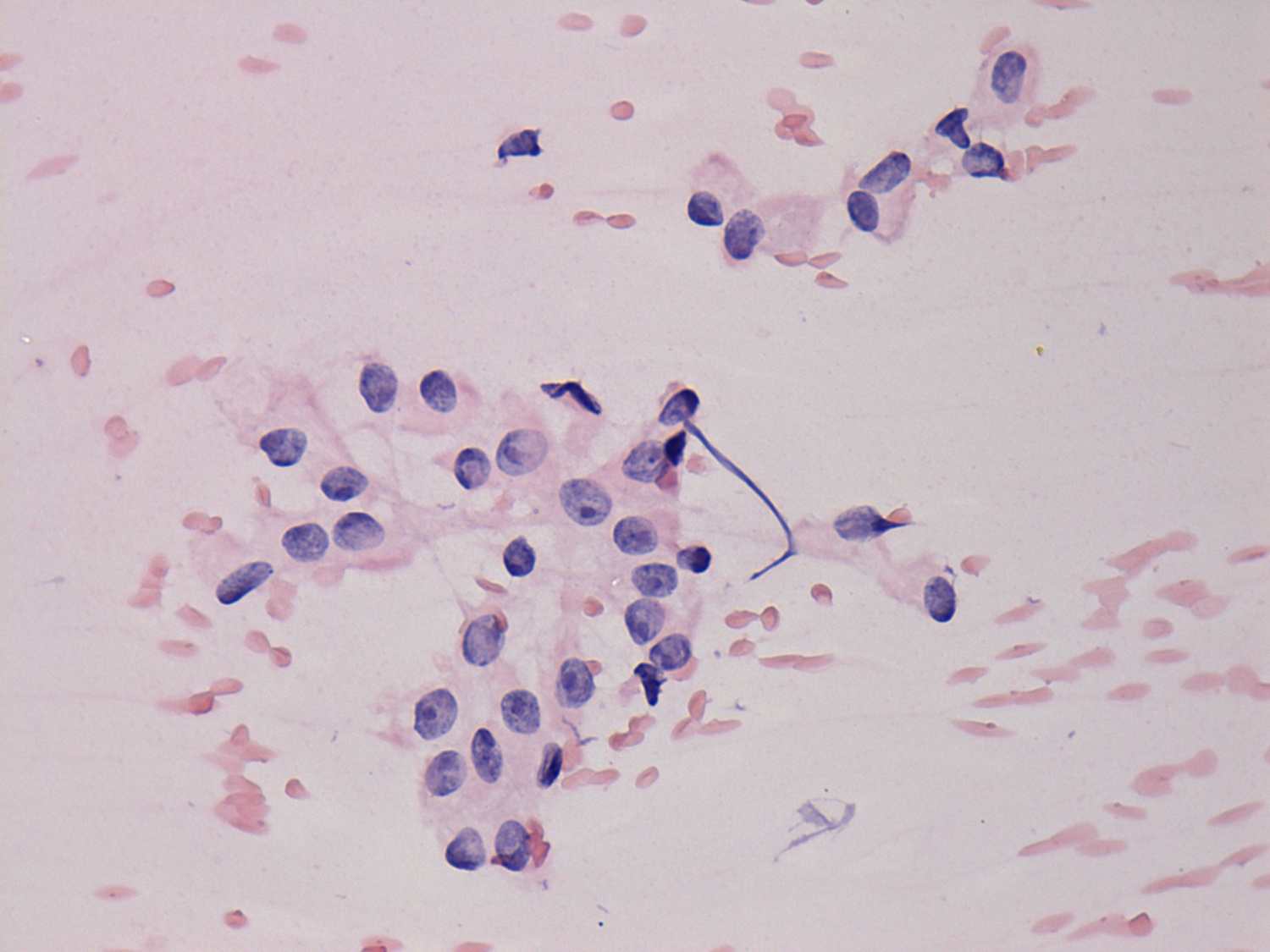
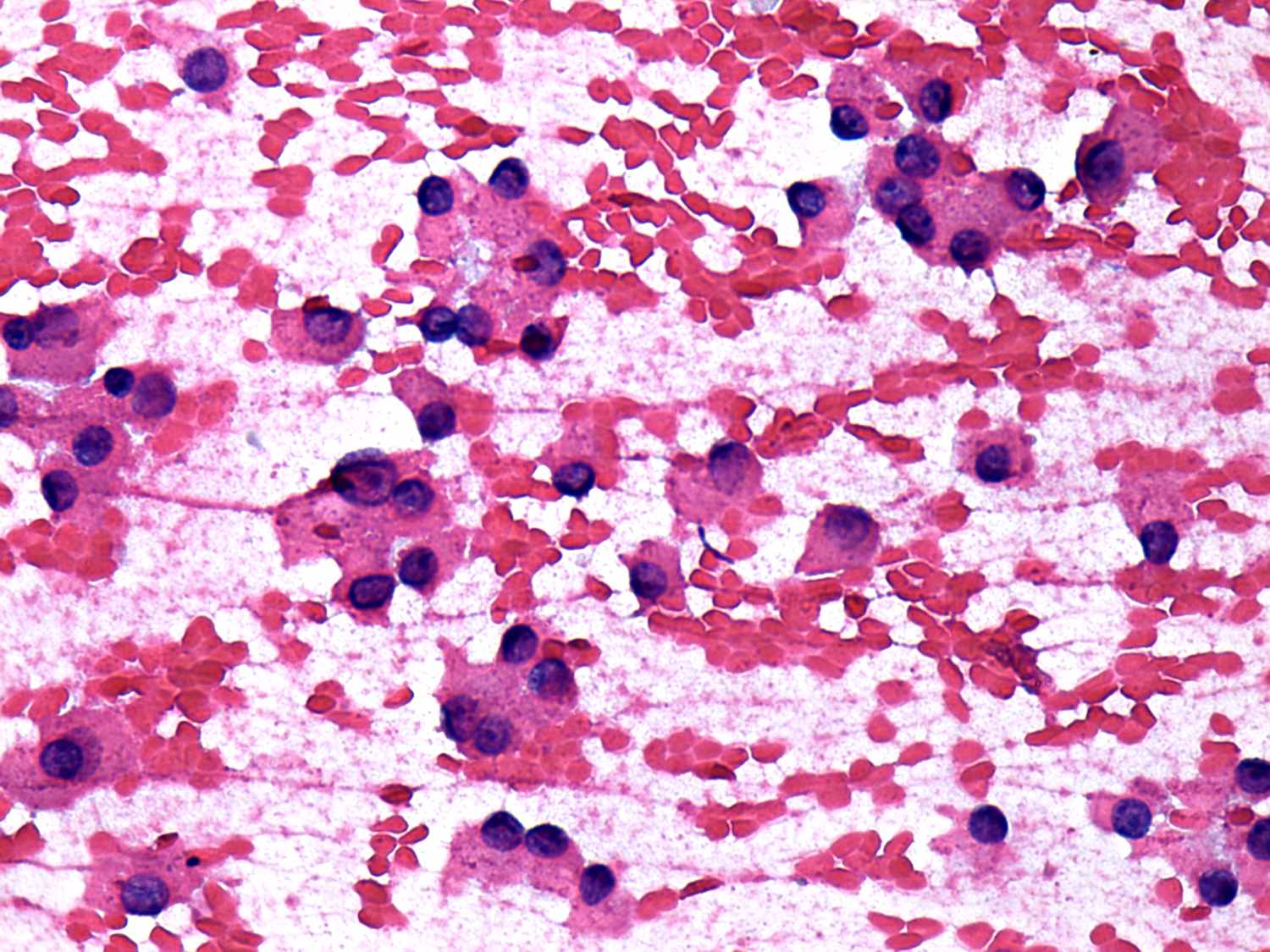
Benign hyperplastic nodule - Case
10 |
|
 |
 |
 |
 |
|
On the presence of dissociated cells, prominent nucleoli and the lack
of colloid, the risk of an oxyphilic tumor is greater than 50%. The
presence of an inclusion has only limited significance in metaplastic
cells.
|
The whole pattern corresponds to a non-tumorous lesion: oxyphilic cells
are mostly in sheets, only a few cells exhibit nucleolus and there is
colloid in the background. The presence of grooves has only limited
significance in metaplastic cells.
|
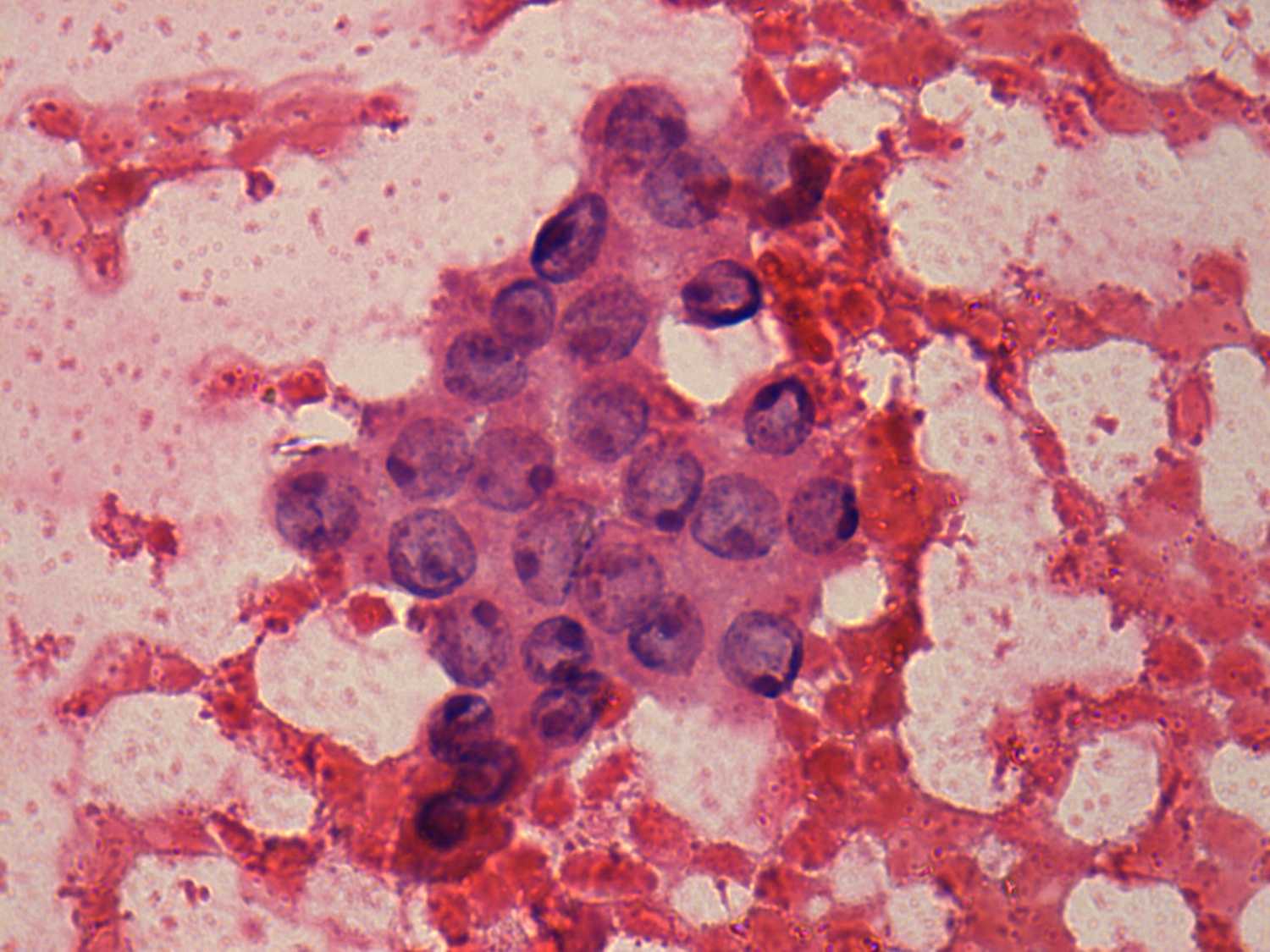
Benign hyperplastic nodule - Case
26 |
|
 |
 |
 |
 |
|
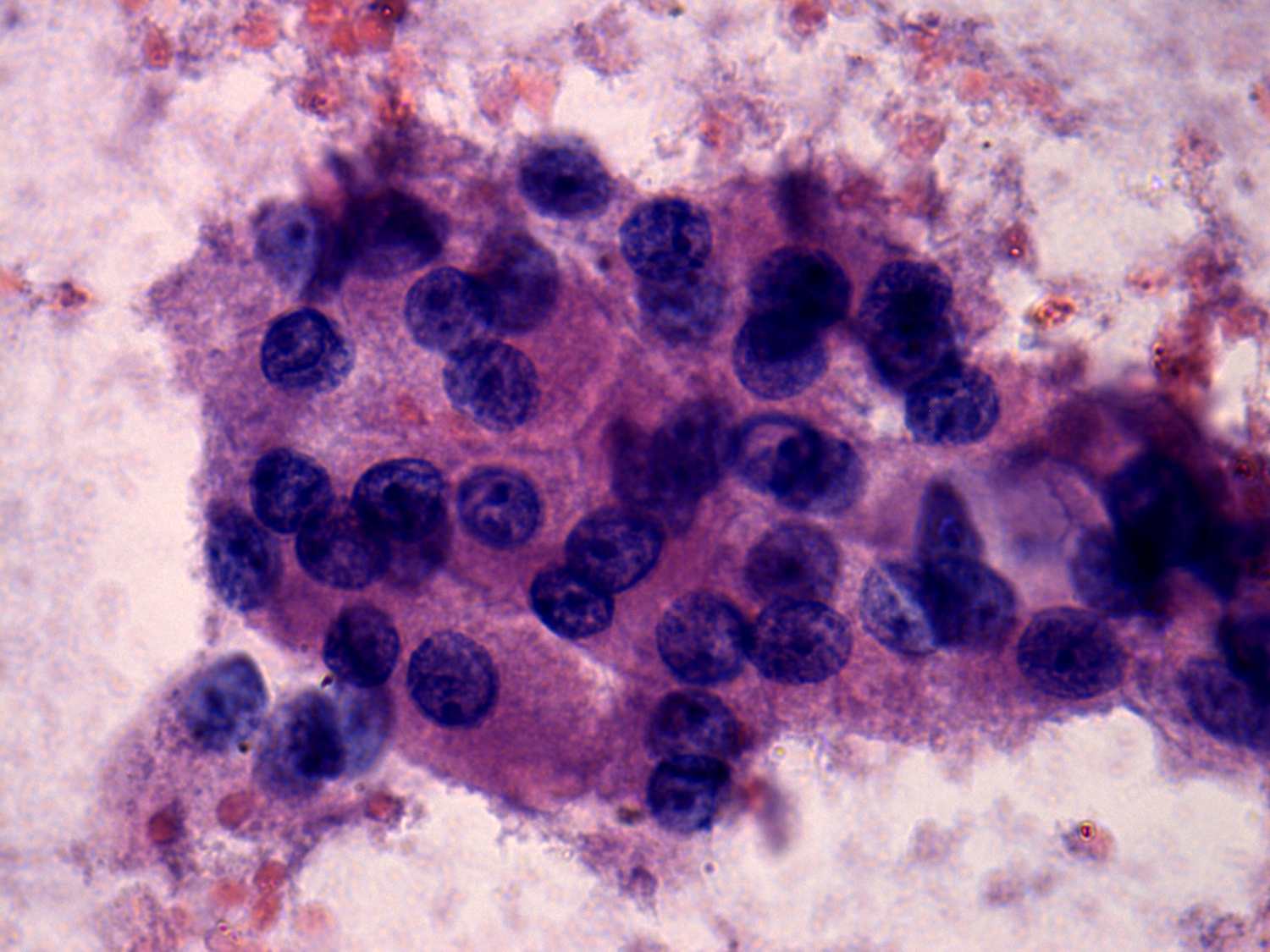
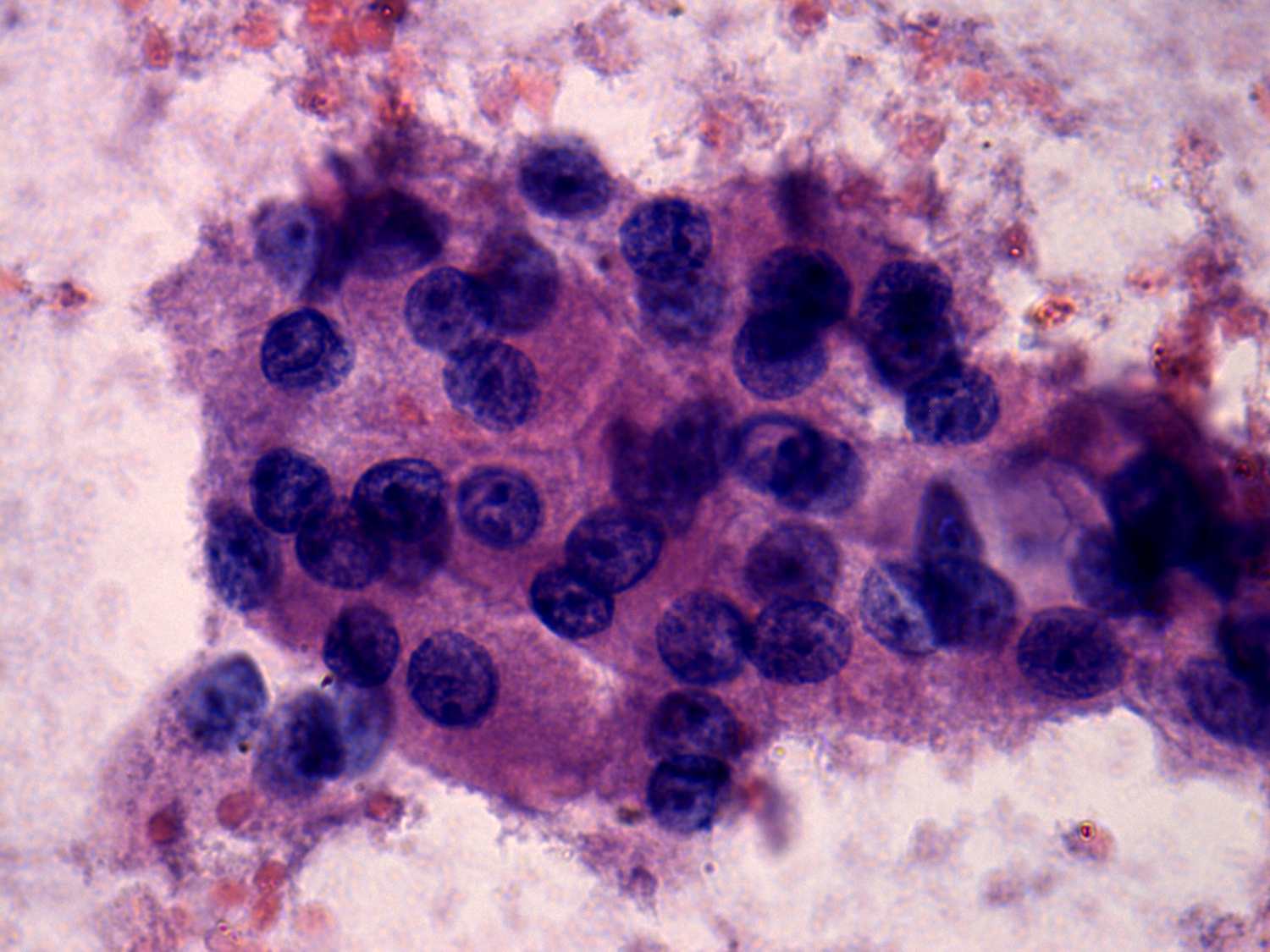
The cytological pattern is identical in these cases: most if not all
thyrocytes exhibit oxyphilic changes, they present prominent nucleoli
and there is an unequivocal tendency of cells to dissociate. The risk
of a Hürthle-cell tumor was much greater than 50% in both cases.
|
Benign hyperplastic nodule - Case
52 |
|
 |
 |
 |
 |
|
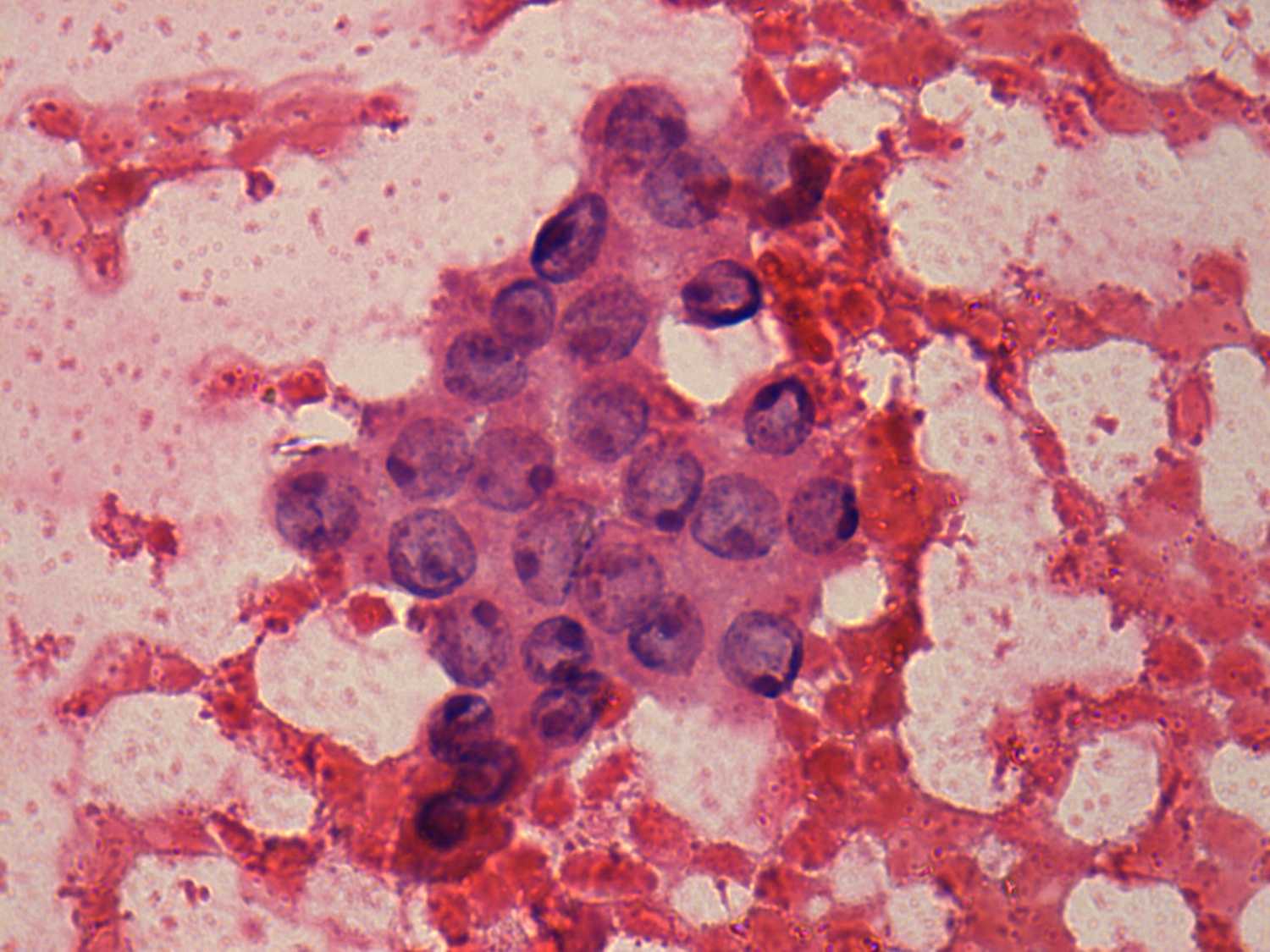
Every cell presents oxyphilic metaplasia, contains large promient
nucleoli and there is no colloid in the background. These properties
raise the possibility of an oxyphilic tumor. On the other hand the lack
of tendency to dissociate stands againts this possibility.
The risk of an oxyphilic tumor (either an adenoma or an oxyphilic variant of follicular cancer) based solely on the cytological pattern was more than 50%.
|
Microfollicular proliferation is more pronounced and tendency of cells
to dissociate can be observed. The risk of an oxyphilic tumor was more
than 80%.
|