|
Lymphocytic thyroiditis |
|
Clinical presentation
Most of the cases belong in one or other of the following groups.
1. Newly-developed hypothyroidism with either an enlarged or an
atrophic thyroid
In those countries where there is not a severe iodine deficiency, LT is
practically the only cause of hypothyroidism, with the exceptions of
postoperative hypothyroidism and the iatrogenic (iodine-induced) form.
The latter conditions are revealed by the patient history. FNAC is
therefore indicated in most cases if the thyroid is enlarged. If US is
performed before FNAC, then clinically misinterpreted or doubtful cases
of nodular form can be excluded. In most cases of the "nodular" form of
Hashimoto's thyroiditis, only pseudonodularization is present. If there
is any doubt as to the benign nature of a nodule, FNAC is mandatory.
2. A hyperthyroid patient without thyroid-associated
ophthalmopathy
The question here is whether hashitoxicosis or Graves-Basedow's disease
is the cause of hyperthyroidism. Subacute LT is best regarded as of
this form, which consists mainly of postpartum thyroiditis.
3. Patients investigated for diffuse or nodular enlargement of the
thyroid (including incidentalomas detected by carotid Doppler or
thyroid US examination)
In most of these cases, a correct FNAC diagnosis of LT can be made. On
the other hand, this can be one of the greatest pitfalls in thyroid
cytology. A great number of hypoechogenic lesions within an echonormal
thyroid belong in this group. Since we are not aware of the possibility
of LT, in cases where pronounced epithelial atypia is present without a
relevant number of lymphocytes, the final FNAC report is not
infrequently indeterminate, resulting in surgery. The situation is
similar in those cases where a nodule is palpable. Besides US
examination, the only chance of avoiding this pitfall is to be aware of
the possibility of it.
4. Differential diagnostics of a painful thyroid
The pain occurring in Hashimoto's thyroiditis is usually mild. The
patients describe it as "tenderness". On the other hand, in certain
cases with a painful clinical presentation, in addition to the frequent
causes (de Quervain's thyroiditis, or a suddenly-developed thyroid
cyst) LT must also be considered. In a small proportion of these cases,
despite a thorough analysis of the clinical and cytological data, we
cannot decide whether the complaint of the patient is caused by a
granulomatous or a chronic lymphocytic form. A follow-up of the patient
will be decisive.
Ultrasonography
Hypoechogenicity of
various degrees is the basic  property
of a chronic lymphocytic thyroiditis (LT). The marked, diffuse hypoechogenic
presentation causes little diagnostic problem – most patients have an
underlying autoimmune disease; de Quervain's thyroiditis is the only
differential-diagnostic problem.
property
of a chronic lymphocytic thyroiditis (LT). The marked, diffuse hypoechogenic
presentation causes little diagnostic problem – most patients have an
underlying autoimmune disease; de Quervain's thyroiditis is the only
differential-diagnostic problem.
The first basic diagnostic problem arises in patients with only minimally or moderately hypoechogenic pattern. If we do not notice this form in a euthyroid patient, our report will result falsely in the case of a healthy thyroid. Conversely, if we notice the hypoechogenicity in a euthyroid patient, we can consider the possibility of the underlying autoimmune thyroid disease and therefore we can give the chance to recognize hypothyroidism later.
The other fundamental
problem is caused by focal hypoechogenicity. This is apparently the
most important differential diagnostic problem in thyroid ultrasound.
To  resolve this
problem with success, it requires a systematic comparison of the
ultrasound pattern with the final diagnosis based on clinical,
laboratory, cytological, in certain cases follow-up results and in
surgically treated patients possibly with the macroscopic and
microscopic pathological findings. To consider LT in each hypoechogenic
pattern - including solitary hypoechogenic lesions - is the most
important rule in thyroid ultrasound. The most important properties in
the differentiation of LT and a nodule in pathological sense are the
following:
resolve this
problem with success, it requires a systematic comparison of the
ultrasound pattern with the final diagnosis based on clinical,
laboratory, cytological, in certain cases follow-up results and in
surgically treated patients possibly with the macroscopic and
microscopic pathological findings. To consider LT in each hypoechogenic
pattern - including solitary hypoechogenic lesions - is the most
important rule in thyroid ultrasound. The most important properties in
the differentiation of LT and a nodule in pathological sense are the
following:
The borders of a lesion
in LT are generally not regularly  geometrical,
but the hypoechogenic area is connected to echonormal parenchyma not
yet influenced by thyroiditis.
geometrical,
but the hypoechogenic area is connected to echonormal parenchyma not
yet influenced by thyroiditis.
In contrast with true nodules or evolving multinodular goiters, in the event of LT we find not one or two but numerous circumscribed areas. Finding less than four hypoechogenic lesions is rare in the case of LT.
If the basic echostructure of the thyroid is not echonormal but minimally or moderately hypoechogenic, the chance of LT is higher.
The size of the thyroid may be also of help. The thyroid is in most cases enlarged in a multinodular goiter. It means that the finding of a not enlarged thyroid in the case of multiple hypoechogenic lesions greatly increases the possibility of LT.
If we have any doubt, we have to raise the possibility of LT on the ultrasound report. The clinical picture, the FNAC and antibody determination will be of help. In a small proportion of patients, even after a complex evaluation, we cannot give an evident diagnosis. The change in US pattern, antibodies, and hormone-levels on follow-up investigations will resolve the problem. We emphasize the well-known close correlation between aTPO level and hypoechogenicity index here. It means that even in the problematic cases, the help of aTPO is only limited.
Thyroid nodules occur in
a similarly large proportion of LT as opposed to non-LT patients. This
pro blem
has been mentioned earlier. We are faced with another special problem in
diffuse hypoechogenicity which may cover a similarly hypoechogenic
nodule. We can recognize such nodules by thorough gray-scale
investigation and by the difference in the vascularization of the
nodular and the non-nodular part of the thyroid.
blem
has been mentioned earlier. We are faced with another special problem in
diffuse hypoechogenicity which may cover a similarly hypoechogenic
nodule. We can recognize such nodules by thorough gray-scale
investigation and by the difference in the vascularization of the
nodular and the non-nodular part of the thyroid.
What about the
hyperechogenic lesions in LT? In contrast
with the previously described situation where we can miss a
hypoechogenic nodule in a hypoechogenic thyroid, in the case of
hyperechogenic lesions, the issue is the overdiagnosis of a nodular
goiter. We must be aware o f
the fact that in LT the secondary and tertiary lobules of a lobe are
more expressed. If we detect a hyperechogenic lesion with a maximal
diameter of 3 to 15 mm, it is more probable that the lesion is only a
secondary lobule than a real one. There are two considerations:
firstly, the term ‘nodule' has to be used only very cautiously.
Secondly, the hyperechogenic lesion in LT means the most frequent
situation where a hyperechogenic nodule may be a focus of a
well-differentiated cancer. If we have any doubt, FNAC is mandatory.
f
the fact that in LT the secondary and tertiary lobules of a lobe are
more expressed. If we detect a hyperechogenic lesion with a maximal
diameter of 3 to 15 mm, it is more probable that the lesion is only a
secondary lobule than a real one. There are two considerations:
firstly, the term ‘nodule' has to be used only very cautiously.
Secondly, the hyperechogenic lesion in LT means the most frequent
situation where a hyperechogenic nodule may be a focus of a
well-differentiated cancer. If we have any doubt, FNAC is mandatory.
 Fibrosis
is a frequent feature in LT. The fibrotic vessels are presented as
bright punctate granules or white lines depending on the angle between
ultrasound and the fibrotic bundle. The misinterpretation of the former
as microcalcification is not a rare situation. It had no negative
consequence in this patient while in the case of a nodule it had.
Fibrosis
is a frequent feature in LT. The fibrotic vessels are presented as
bright punctate granules or white lines depending on the angle between
ultrasound and the fibrotic bundle. The misinterpretation of the former
as microcalcification is not a rare situation. It had no negative
consequence in this patient while in the case of a nodule it had.
Vascularization in LT
In everyday practice,
the vascularization has only limited role in LT. Similarly to the  gray
scale pattern the vascularization is also very diverse in contrast to
the hypoechogenicity on gray scale mode; there is no specific vascular
pattern.
gray
scale pattern the vascularization is also very diverse in contrast to
the hypoechogenicity on gray scale mode; there is no specific vascular
pattern.
Increased blood flow is observed most frequently in the so-called hypertrophic phase of Hashimoto's thyroiditis with hypothyroidism and an elevated TSH-level. There are several special circumstances when the determination of blood flow may have significance. The decreased vascularization is almost decisive in a hyperthyroid patient; this patient has thyroiditis with great probability. Another example is the differential diagnostic problem of circumscribed lesions. The difference in vascular pattern between the lesion and the extralesional part of the thyroid is a sign suggesting different pathological entities.
Sonographic follow-up of patients with LT
 Generally, repeated US
examination has only very limited importance in LT. Except for
post partum thyroiditis, the sonographic pattern in LT changes slowly
over decades and years. Nevertheless, the size of the thyroid correlates well with the TSH level, therefore an
enlarged thyroid in the hypothyroid will become smaller as the TSH level decreases within months or a year.
Otherwise there is a tendency to become the thyroid atrophic over decades. As the thyroid decreases and became atrophic,
the degree of hypoe
Generally, repeated US
examination has only very limited importance in LT. Except for
post partum thyroiditis, the sonographic pattern in LT changes slowly
over decades and years. Nevertheless, the size of the thyroid correlates well with the TSH level, therefore an
enlarged thyroid in the hypothyroid will become smaller as the TSH level decreases within months or a year.
Otherwise there is a tendency to become the thyroid atrophic over decades. As the thyroid decreases and became atrophic,
the degree of hypoe  chogenicity
slowly decreases. Therefore, we have the
chance to detect a hypoechogenic nodule missed on the first examination
because of the similarity of the echogenicity of the nodule and the
extranodular part. This is rather a theoretical possibility.
chogenicity
slowly decreases. Therefore, we have the
chance to detect a hypoechogenic nodule missed on the first examination
because of the similarity of the echogenicity of the nodule and the
extranodular part. This is rather a theoretical possibility.
From a practical point of view, repeated US is necessary in those patients who have focal alterations raising the possibility that the lesion would be a nodule in pathological sense. In patients with enlarged thyroid, the follow-up US examination is suitable to detect changes in size. Naturally, patients with coexistent nodular goiter and LT require regular follow-up US examination.
Cytology
Typical picture
-
Lymphoid cells, including blasts, plasma cells and
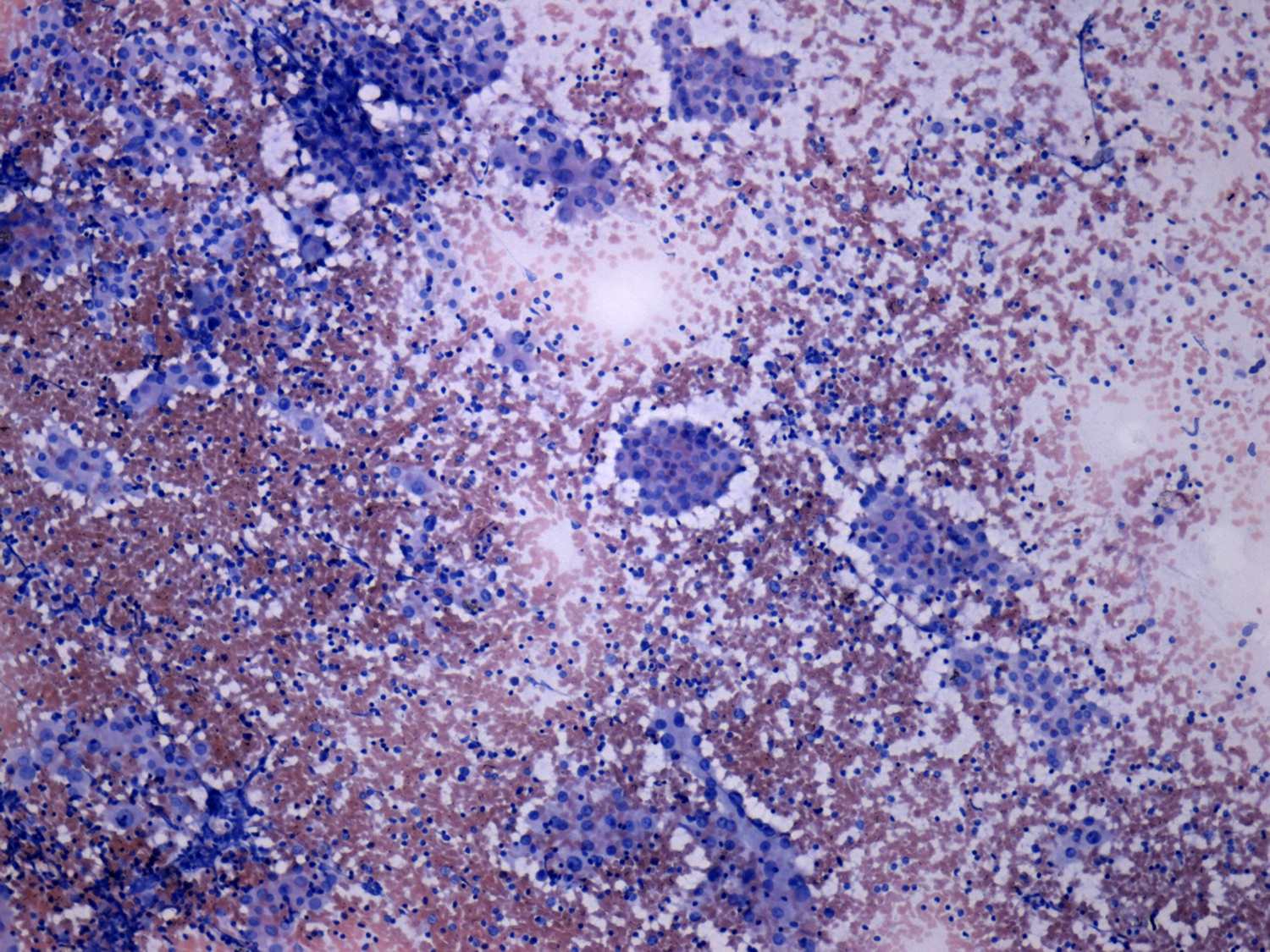 germinal center cells.
germinal center cells.
- Follicular epithelial cells with varying degrees of degenerative changes and/or oxyphilic (= oncocytic = Ashkenazy-cell = Hürthle-cell) metaplasia. The latter may present in a highly atypical, even polymorphic form.
- No or only a minimal colloid in the background.
The presence of atypical
cells is a very frequent finding in LT. Both the thyroiditis itself  and
the dysfunction may cause not only anisonucleosis but even pleomorphism. The degree of the
latter may reach that observed in the case of anaplastic carcinoma.
Nevertheless, if we take the ultrasound and clinical presentation into
account atypia and even pleomorphism cause rarely differential
diagnostic problems.
and
the dysfunction may cause not only anisonucleosis but even pleomorphism. The degree of the
latter may reach that observed in the case of anaplastic carcinoma.
Nevertheless, if we take the ultrasound and clinical presentation into
account atypia and even pleomorphism cause rarely differential
diagnostic problems.
More serious
differential diagnostic problem arises in the presence of inclusion and
grooves. T he
positive predictive value of these intranuclear figures is
limited in the case of thyroiditis therefore the diagnosis of a
concomitant papillary carcinoma is a great challenge for the
cytopathologist is certain cases. The details are presented in section
Papillary carcinoma.
he
positive predictive value of these intranuclear figures is
limited in the case of thyroiditis therefore the diagnosis of a
concomitant papillary carcinoma is a great challenge for the
cytopathologist is certain cases. The details are presented in section
Papillary carcinoma.
Differential diagnostics - cases without oncological significance
Differentiation
from nodular goiter The presence of naked follicular cells in
great number without structure formation may cause problems concerning
the origin of these cells. They may be misinterpreted as small
lymphocytes. The presence or absence of lymphoblast, and the absence or
abundant presence of colloid are of great help.
The other problem is the focal LT near nodular goiters. In these cases,
only scattered lymphocytes are present on the smear. In a small
proportion of the follicular cells, oxyphilic changes may be observed.
The problem is that the term focal LT may be used correctly only on
histopathological reports. If we see the above-mentioned cytological
picture, we cannot exclude the possibility of the presence of typical,
diffuse LT. A clear distinction is not of great relevance. These
patients present with nodular goiter, and therefore either go on to
surgery if the nodule is large and causes compression signs, or will be
monitored because of the nodule.
Differentiation from Graves' disease Both LT (Hashimoto's thyroiditis) and Graves-Basedow's disease belong in the common autoimmune thyroid disease group. They may be separate entities, but may represent two ends of a common disorder. From a clinical aspect in
most cases they are clearly distinct entities, while
in the remaining cases the clinician expects us to categorize them in
one group or the other. The problematic cases are those with a mild to
moderate degree of hyperthyroidism and without significant TAO.  Some
clinicians are influenced by the presence or
absence of thyroiditis in deciding whether to manage the patient with
specific anti-thyroid drugs or not. Antibodies are of limited help in
these cases. And we are of the opinion that the cytological report has
also its limitations. See TABLE.
Some
clinicians are influenced by the presence or
absence of thyroiditis in deciding whether to manage the patient with
specific anti-thyroid drugs or not. Antibodies are of limited help in
these cases. And we are of the opinion that the cytological report has
also its limitations. See TABLE.
Differentiation
from de Quervain's thyroiditis. In most cases, both the
cytological picture and the clinical data on the patient are clear.
While chronic LT may  present
with various clinical pictures, subacute
thyroiditis is manifested in more than 90% of the cases with a highly
specific clinical picture: fever, a hard, uneven consistency and a
painful enlargement of the thyroid, with the ESR above 60 mm/h. In a
few cases, it is very difficult or even impossible to make a clear
distinction between the two type of thyroiditis (Kakudo 1987,
Jayaram 1989b, Jayaram 1990). In our
practice, besides more than 15,000 Hashimoto's thyroiditis, 609
subacute de Quervain's thyroiditis and 872 subacute silent lymphocytic
thyroiditis cases, there were 60 cases where we could not decide on the
type of the underlying disease at the first examination. On follow-up
examinations, complete normalization of the US pattern favours the
diagnosis of previous de Quervain's thyroiditis (this occurred in 9 of
60 cases), while persistent hypothyroidism is seen only in cases of
lymphocytic thyroiditis (31 of 60 cases). 11 of 60 patients gave a
clinical picture involving recurrent attacks of fever, and neck pain
over 3 and 5 years, respectively. Steroid therapy, which has a dramatic
benefit on patients with de Quervain's thyroiditis, had no effect in
these cases. We have no clear-cut evidence, but in our opinion these
cases are a form of LT.
present
with various clinical pictures, subacute
thyroiditis is manifested in more than 90% of the cases with a highly
specific clinical picture: fever, a hard, uneven consistency and a
painful enlargement of the thyroid, with the ESR above 60 mm/h. In a
few cases, it is very difficult or even impossible to make a clear
distinction between the two type of thyroiditis (Kakudo 1987,
Jayaram 1989b, Jayaram 1990). In our
practice, besides more than 15,000 Hashimoto's thyroiditis, 609
subacute de Quervain's thyroiditis and 872 subacute silent lymphocytic
thyroiditis cases, there were 60 cases where we could not decide on the
type of the underlying disease at the first examination. On follow-up
examinations, complete normalization of the US pattern favours the
diagnosis of previous de Quervain's thyroiditis (this occurred in 9 of
60 cases), while persistent hypothyroidism is seen only in cases of
lymphocytic thyroiditis (31 of 60 cases). 11 of 60 patients gave a
clinical picture involving recurrent attacks of fever, and neck pain
over 3 and 5 years, respectively. Steroid therapy, which has a dramatic
benefit on patients with de Quervain's thyroiditis, had no effect in
these cases. We have no clear-cut evidence, but in our opinion these
cases are a form of LT.
As mentioned above, in our practice a FNAC report is not a
morphological, but a clinical cytological diagnosis. Thus, if the
clinical picture is clear (a patient either with highly elevated titers
of thyroid autoantibodies or with a classical presentation of subacute
thyroiditis), the absence of either of the typical elements of the
cytological picture is not of great relevance.
If the cytological picture is not decisive, and we are faced with a
patient who has malaise, while the clinical picture only resembles, but
is not typical of subacute thyroiditis (only subfebrility, and the ESR
is not highly elevated), we treat the patient as having subacute
thyroiditis. We monitor the clinical data and the US picture of the
patient very closely. One year later, we have been able to make a
clear decision in all of our cases where there was an original doubt or
failure. At this time, the US findings will be quite normal in cases of
subacute thyroiditis, while in cases of LT, diffuse hypoechogenicity
will remain.
Differential diagnostics - cases with oncological significance
Lymphocytic
thyroiditis or MALT-type lymphoma? This problem is well known
from the literature ( Kini 1981, Kini 1987 ). MALT lymphomas
of the thyroid evolve on the basis of underlying Hashimoto's
thyroiditis. In our practice, differentiation of the two entities
caused a great problem only exceptionally. We again emphasize the role
of the clinical data in making a clinical cytological diagnosis. MALT
lymphoma of the thyroid has a typical clinical appearance. The patient
is 60 years old or more. The thyroid becomes enlarged quite rapidly
(within 2 months) and is hard, and US reveals a diffuse hypoechogenic
pattern. All of these four features may be seen together in only very
few cases of Hashimoto's thyroiditis; in our practice, it has occurred
in only less than 1% of patients with Hashimoto's thyroiditis.
Hashimoto's thyroiditis may present as a diffuse goiter that develops
rapidly in younger patients, but in the elderly it is a
slowly-developing disease. In those cases where a differentiation
between the two diseases is not possible, immunocytochemical staining
is recommended (Rosai 1992), while malignancy cannot be ruled
out even on the basis of the polyclonal nature of the lesion. Those
cases where a monoclonal tumor population is present belong in the
group of lesions where routinely-stained smears are also informative.
On the other hand, in 3 of our first 6 patients with MALT thyroid
lymphoma the cytological picture w as
difficult to interpret as
malignant. It rather resembled those observed in florid LT, which
characteristically occurs in younger patients (Orell 1987). A
heterogeneous lymphoid population may be seen in combination with
scattered follicular cells of oxyphilic type. However, all of the
patients were above 60, and had an extremely diffuse goiter that had
developed very rapidly. Two of the 3 patients had stridor and dyspnea
at rest. This suggested the possibility of MALT lymphoma associated
with Hashimoto's disease. To date neither false-positive (including
suspicious results) nor false-negative reports of thyroid lymphoma have
been made.
as
difficult to interpret as
malignant. It rather resembled those observed in florid LT, which
characteristically occurs in younger patients (Orell 1987). A
heterogeneous lymphoid population may be seen in combination with
scattered follicular cells of oxyphilic type. However, all of the
patients were above 60, and had an extremely diffuse goiter that had
developed very rapidly. Two of the 3 patients had stridor and dyspnea
at rest. This suggested the possibility of MALT lymphoma associated
with Hashimoto's disease. To date neither false-positive (including
suspicious results) nor false-negative reports of thyroid lymphoma have
been made.
Lymphocytic
thyroiditis or Hürthle-cell tumor? There is a well-known
pitfall in thyroid cytology here (Guarda 1987, Kini 1987, Gonzalez
1993, Nguyen 1997). The microscopic picture is that oncocytes are
the predominant cells, but a number of scattered lymphocytes are also
seen.
The presence of large nucleoli, and the loosely arranged pattern of
oncocytes with many dispersed cells is characteristic of the tumorous
origin of the lesion. On the other hand a lack of nucleoli or a lack of
dispersed cells favours a non-tumorous origin (Ravinsky 1988).
Despite these cytological signs, in most of the cases we are not able
to make a clear-cut distinction between the two possibilities, and
surgery is therefore the most frequent treatment of choice (Nguyen
1997).
Again the role of US is emphasized. If we see a well-circumscribed
lesion within an absolutely echonormal background, the possibility of a
tumor is greatly enhanced, whereas a more hypoechogenic lesion is much
less likely to be of a tumorous nature. In our practice, the decision
as to whether to operate on a patient or not is based on four
parameters: the cytological picture, the US findings (both the pattern
outside the nodule and that of the lesion itself), the size of the
lesion, and the compliance of the patient. (See TABLE) In a number of
cases, we perform repeated
aspirations on the nodule. If these show the characteristic picture of
Hashimoto's thyroiditis, this can be of great help in avoiding
unnecessary surgery. Another opportunity must
be borne in mind when we make a decision on the basis of the results of
one examination. Under special, but not rare circumstances, we offer
follow-up examinations 6-12 months later for the patients instead of
sending them for operation on the basis of one examination procedure
with indeterminate results. Two other very important parameters may be
analyzed if we have results from two different occasions. First, the
change in size of the nodule, and second, the change in the sonographic
pattern of the thyroid outside the nodule. As revealed by Table 5, many
unnecessary operations can be avoided in this way. TABLE
Other factors are of limited importance in this field. The  determination
of autoantibody levels has been suggested (Baker 1983).
On the other hand, LT is also present near many Hurthle-cell tumors.
Elevated titers of thyroid autoantibodies, therefore do not exclude the
possibility of a concomitant Hurthle-cell tumor. Physical examination
also has limitations in these cases. The hard consistency of a nodule
is a sign which favours a tumor rather than a non-tumorous lesion, and
also favours a malignant rather than a benign tumor. This is the case
when LT can be excluded. However, in LT most of the palpable nodules
are firm, irrespective of their tumorous or non-tumorous origin. In an
earlier period of our practice, when we did not perform US, in 5 cases
we sent a patient for surgery, but histopathology revealed Hashimoto's
thyroiditis in a thyroid without any nodule. These palpable lesions
were small, and the cytological picture was that described above:
predominantly of Hurthle-cell type with a number of scattered or no
lymphocytes. Our experience with these 5 patients also demonstrates the
role of US. If we see a picture resembling well-differentiated
epithelial tumor, but the US shows no lesions in the part of the
thyroid in question, a tumor can be excluded, even if a lesion is
palpable. A palpable lesion without a US difference can not be a
well-differentiated epithelial tumor.
determination
of autoantibody levels has been suggested (Baker 1983).
On the other hand, LT is also present near many Hurthle-cell tumors.
Elevated titers of thyroid autoantibodies, therefore do not exclude the
possibility of a concomitant Hurthle-cell tumor. Physical examination
also has limitations in these cases. The hard consistency of a nodule
is a sign which favours a tumor rather than a non-tumorous lesion, and
also favours a malignant rather than a benign tumor. This is the case
when LT can be excluded. However, in LT most of the palpable nodules
are firm, irrespective of their tumorous or non-tumorous origin. In an
earlier period of our practice, when we did not perform US, in 5 cases
we sent a patient for surgery, but histopathology revealed Hashimoto's
thyroiditis in a thyroid without any nodule. These palpable lesions
were small, and the cytological picture was that described above:
predominantly of Hurthle-cell type with a number of scattered or no
lymphocytes. Our experience with these 5 patients also demonstrates the
role of US. If we see a picture resembling well-differentiated
epithelial tumor, but the US shows no lesions in the part of the
thyroid in question, a tumor can be excluded, even if a lesion is
palpable. A palpable lesion without a US difference can not be a
well-differentiated epithelial tumor.
Diagnosing a
follicular tumor in patients with lymphocytic thyroiditis.
Besides the well-known concern about follicular tumors, another aspect
of this  problem
arises in patients with LT. The misinterpretation of
thyroiditis-related cell changes as follicular neoplasia is a frequent
problem (Carson 1996). A cytologic differentiation between
Hashimoto's thyroiditis and follicular tumor is therefore impossible in
some cases (Nguyen 1997). On the other hand, if we are aware
about the US picture, we can avoid unnecessary surgical explorations in
those patients where only pseudonodularity exists.
problem
arises in patients with LT. The misinterpretation of
thyroiditis-related cell changes as follicular neoplasia is a frequent
problem (Carson 1996). A cytologic differentiation between
Hashimoto's thyroiditis and follicular tumor is therefore impossible in
some cases (Nguyen 1997). On the other hand, if we are aware
about the US picture, we can avoid unnecessary surgical explorations in
those patients where only pseudonodularity exists.
Lymphocytic thyroiditis or papillary carcinoma? See Chapter on papillary carcinoma.
